Learning Objectives
This is an intermediate-level course.
After completing it, mental health professionals will be able to:
- Identify
transference and countertransference as they manifest themselves in therapy.
- Describe the five
tasks and the self-monitoring function therapists must perform in order to use transference and countertransference benevolently.
- Formulate efficacious
transference and countertransference interpretations.
- Explain when, with
whom, and how frequently to use transference and countertransference
interpretations.
This course is based on the most accurate
information available to the author at the time of writing. Cognitive
psychology and neuroscience findings regarding brain development, structures,
and activities continue to shed light on what were once regarded as merely
psychoanalytic concepts and processes. Consequently, new information may
emerge that supersedes some explanations in this course.
This course may provoke disturbing
feelings in readers due to their unresolved conflicts, but it also gives them
information about processes by which they can resolve these conflicts.
Outline
- Introduction
- Manifestations of Transference and Countertransference
- Challenges Inherent in Identifying Transference and Countertransference
- Words: Therapeutic Material
- Words: Extra-therapeutic Material
- Vocal Bursts
- Feelings: Transferential
- Feelings: Countertransferential
- Dreams
- Fantasies and Daydreams
- Behavior
- Diagnostic and Interpretive Tasks
- First Task: Taking In Transferred Material
- Second Task: Holding and Permitting Regression
- Third Task: Decoding
- Fourth Task: Formulating Hypotheses
- Fifth Task: Verifying Hypotheses
- Overarching Meta-Function: Self-Monitoring
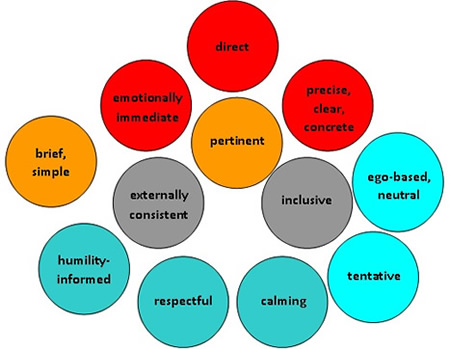
- Wording Transference and Countertransference Interpretations
- A Transference Interpretation
- A Countertransference Interpretation
- The Right Attitude
- Qualities of Effective TRIs and CTRIs
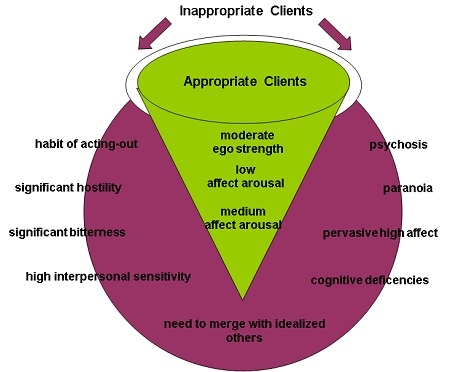
- Using Transference and Countertransference Interpretations
- Appropriate Versus Inappropriate Clients
- Timing
- Frequency
- Principles Underlying Guidelines for Using TRIs and CTRIs
- Final Thoughts
- Footnotes
- References
Introduction
Transference and countertransference can contribute to positive therapeutic outcome in non-analytic therapy as much
as in analytic therapy. They can also contribute to negative outcome and
treatment failure. If existential, cognitive-behavioral, or any other non-analytically
oriented therapists fail to notice these displaced phenomena at work in their
sessions, they are limited in their ability to help their clients move beyond
their one-sided perceptions of the problematic relationships and events they
experience both outside of therapy and in therapy. “Extant empirical work
supports” (Gelso & Bahatia, 2012, 388) this conclusion (Buchheim et al., 2017; Tmej et al, 2020; Antichi & Giannini, 2022).
If, however, therapists identify and
decode displaced material that manifests itself during therapy, they
can complement and/or correct clients’ perceptions. Then, as therapists share their insights and invite corroboration, clients can consider how what is transpiring in therapy is the result of their unresolved conflicts and explore appropriate ways of resolving them. Thus they can heal themselves and engage in wholesome relationships with others.
This course explores how transference and countertransference manifest themselves in subtle ways that therapists can learn to identify and use to enlighten clients regarding their contribution to their interpersonal difficulties. This course also teaches clinicians to identify the covert ways in which they are contributing to the interactions they are having with their clients. It also sensitizes clinicians to transcultural and intracultural mediators and moderators of transference and countertransference manifestations.
Finally, this course outlines the five tasks of diagnosing and interpreting transference and countertransference and clarifies therapists’ need to monitor their work as they perform these tasks. It helps them identify clients who will benefit from this interpretive work at appropriate times during their sessions.
This is the second course in a three-part series, based on Transference and Countertransference in Non-Analytic Therapy: Double-Edged Swords by Judith A. Schaeffer, Ph.D. (Lanham, MD: University Press of America, 2007).
The third course focuses on how to benefit from transference and countertransference love that arises in therapy.
(Note: To return to the course after clicking a footnote, click the Back button in your browser.)
Manifestations of Transference and Countertransference
Challenges Inherent in Identifying
Transference and Countertransference
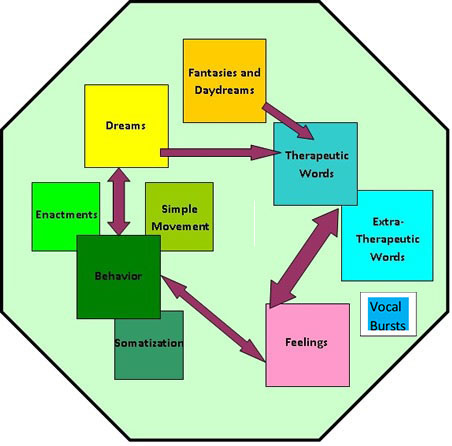
Transference and countertransference
challenge therapists in at least three ways. First, because the conscious mind
cannot have direct knowledge of phenomena “residing” in the unconscious mind,
therapists can detect transferred material only in the vague, shadowy
signs of its presence. They can discover it only as it manifests itself in
words, feelings, dreams, fantasies, somatic responses, and behavior; as each of
“these voiceless and vociferous little parts of [the self] … do their best to
add their ‘two cents’ to the final product” (Wittig, 2002, 143).
Second, because manifestations of
transference and countertransference are a source of data but not a
source of evidence (Smith, 1990), therapists cannot simply take them at
face value. They suggest what is probably going on but cannot be used in
and of themselves to prove what is going on. Consequently, therapists
must “unpack” them for them to yield the information they hold. Especially
in the case of traumatized clients, Ogle and colleagues (2013) warn, therapists
must subject manifestations to decoding and interpretation.
Third, therapists must not forget that
transferred material is characterized both by similarities across cultures and
differences among and within cultures. Roles of women, for instance, are similar yet
distinctive in Islam and Christianity or in the eyes of adolescents versus senior citizens. Hence, therapists must attend to transcultural as well as
intracultural variables in order to discover the most likely meaning of transference
and countertransference phenomena.
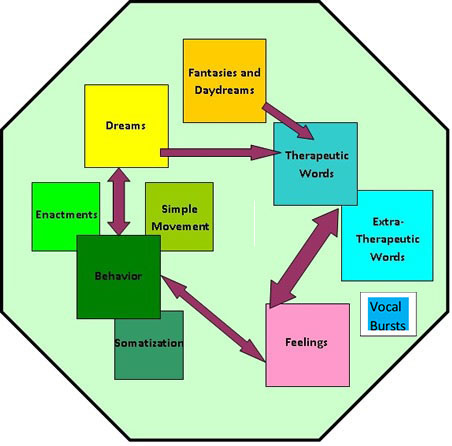
Categories of transference and
countertransference manifestations are artificial in one respect because they
overlap and merge. Emotions, for example, find expression in words, facial
expressions, gestures, and dreams even as dreams consist primarily of actions
taht evoke affect. Examining these categories separately, however, permits us
to simplify complex phenomena and create manageable templates that can be
placed over what transpires in and between therapy sessions.
Words: Therapeutic Material
Most therapists want to believe that the words clients use validly and reliably reveal the true nature of their problems and concerns. Thus therapists take these words at face value. They use their denotations or dictionary definitions.
However, many words with denotations clients consciously use to convey meaning also carry connotations or affective associations of which they may be unaware. Many convey meaning laden with subtle, emotional nuances. A client who says that she wants to work on her relationship with her father, for example, may simply mean her biological father. But she may also be unconsciously revealing her need to improve her relationship with others she associates with that man: those in authority, those who protect her, or those who are simply older and male. The client may even be referring to her older, noticeably self-confident, take-charge female therapist.
Similarly, a client who says, “I want to get rid of my depression” may mean “my sadness, loneliness, and listlessness.” But she may also be unconsciously referring to the depressing quality of her therapeutic relationship that closely resembles interactions with her self-centered spouse.
Thus therapists must be open to the possibility that connotation-bearing words that clients use are manifestations of transference. They are “messages” from the unconscious mind. They are Freudian “slips.”
Therapists should suspect the same of what they themselves say because the unconscious mind is always trying to find ways to move its contents into consciousness. Therapists unintentionally say what they consciously forbid themselves to say. “I am afraid I cannot schedule you next week,” for example, may be revealing therapists’ fear of what clients are about to share with them.
1
Words: Extra-therapeutic Material
Therapists intent on discovering transference must also examine the seemingly irrelevant material that clients introduce in sessions. At times, in referring to extraneous material, clients are consciously intending to shed light on their goals, give background material, or provide information about themselves. At other times, however, clients are unconsciously revealing the nature of their therapeutic relationship (Kahn, 1997). They might be trying to reveal what is hindering their progress in therapy.2
Despite the
client’s clearly stated goal to learn to be a better parent, she began her
second session by speaking of not being called back to substitute teach by a
local school. She wondered if she had not done a good enough job. Her
therapist, in turn, wondered whether his client was really asking about how
well she had done during her first session. Had her performance been good
enough for her therapist?
The therapist
remembered that his client had called that morning to ask about the roads.
Because heavy rains had made roads slick near her house, she wondered whether
he thought the roads near his office were dangerous. She really
wondered whether her therapist would call her again, so to speak, or be like
the school personnel. Was it dangerous to travel the “road” to therapeutic
work?
The therapist decided to test his hypothesis that the call the client made to him was due less to the weather than to her concern about his evaluation of their first session. He began the session by asking, “Did I seem disappointed in our session? Did you call to find out how emotionally dangerous it might be to come back?”
The client
breathed a sigh of relief and answered thoughtfully. Yes, there were
similarities between him and school personnel. He too was an evaluator who
might find her wanting. Yes, it felt dangerous to her to think of returning.
Subsequently, she
returned weekly, revealing in detail how her early years were marked by poor
grades for performance in the “book” of her father. Then she dealt with feeling
inferior as a parent and teacher.
As this vignette reveals, when talking
about a third party, clients may be displacing toward their therapist.
They may be unintentionally revealing their feelings about the person with whom
they are working and sides of themselves they might safely reveal during their
sessions.
Clients’ urge to do so – to reveal
self-in-relationship – is unusually strong in the closeness of the therapeutic
setting. For it is there that their unconscious desire to share what is really
important, but too threatening, most easily breaks through the barrier between
the conscious and unconscious minds. It is “intended” on an unconscious level.3
The client complained
bitterly of his religion teacher, saying how stupid and “out-of-it” she was. He
could not stand her or her class. His cognitive-behavioral therapist listened
attentively, waiting for an opportunity to help her client recognize the value
of doing his assignments for the class despite of his feelings toward his
teacher. Not doing homework and skipping class were the client’s presenting
problems. Though he was bright and capable, he was failing.
One morning, a frantic call from the client’s mother exposed his drug problem. He had been expelled from school for smoking marijuana, and it was not the first time. Realizing she should have decoded his hatred-for-his-teacher remarks much sooner, the therapist said, “You never even mentioned you were having trouble with drugs.” Her client looked painfully embarrassed but quickly shot back with, “I can’t talk to you about certain things. You’re too old. You don’t understand what it’s like to be me.”
Too late, far too late, had the client’s real message become clear. Had the therapist decoded the transferential meaning of his complaints about his teacher, she could have afforded him an opportunity to explore his belief that closeness in age was a prerequisite for trusting a person. Without that, he could only presume that his therapist was as much “out-of-it” as his teacher. He could not count on his therapist to understand his pain.
Especially noteworthy is extra-therapeutic material that clients bring in at the beginning or end of sessions. Seemingly unconnected to hardcore therapeutic work, it often holds important transferential messages.
He walked in
feeling very, very tired, saying he couldn’t get enough sleep. “Was he also
saying that he was very tired of therapeutic work?” his therapist wondered. Was
his therapist’s insistence on his becoming self-sufficient tiresome for him although it was his stated goal?
“Maybe,” the
client answered when asked about possible in-session fatigue. “I am tired of
people trying to change me,” he admitted. “It started back in grade school. The
teachers always had something hard for me to learn. It seemed it would ever
end.” Then, after a brief period of silence, he breathed a sigh of relief,
saying “Nobody ever cared about how hard it was for me before today.”
Subsequently he moved with uncharacteristic zeal into what he himself needed to
change.
Vocal Bursts
Transference can also be manifested in what
are called vocal bursts: “brief linguistic sounds that occur in between
[words] in the absence of speech” (Cowen et al., 2019, 699), such as sighs, gasps,
and laughs. These pre-language, trans-cultural vocalizations indicate some 13
emotions, including awe, disgust, contentment, and ecstasy. Thus therapists
identifying transference cannot afford to ignore them.
Feelings: Transferential
Transferential feelings are those
displaced to the therapist because of subtle similarities between the therapist
and persons outside of therapy. Clients whose parents were intolerant of them,
for example, may experience their therapist as intolerant because of displaced
feelings triggered by a “kernel of truth:” the therapist’s subtle but intolerant behavior.4
Though single, obvious feelings would not
appear to require decoding, what appears to be a simple feeling may indeed be an
emotional blend: a complex emotion with a second or even third feeling at the
periphery of the obvious one (Cowen et al., 2019). Anger due to a therapist
being slightly intolerant, for example, may include fear of the therapist’s
rejection and sadness because of it.
“She cancels for
so many reasons,” her therapist thought. Some seem legitimate, others flimsy. She
recognized that the material on which the client was working was embarrassing
for her, but she wondered whether their therapeutic relationship was even more of
an obstacle to her coming?
When her client
finally came for a session, the therapist listened and watched for displaced
material that might help her decode what on the surface appeared to be positive
feelings. She also opened herself to decoding her own countertransference:
annoyance that sessions were being cancelled and fear of a premature
termination.
Finally, when her
client described her mother-in-law as controlling and said she was going to set
firm limits with her, the therapist decided to use a transference
interpretation to ask if her client felt able to set limits during sessions.
Her client said that she wasn’t sure. Noting that ambivalence, however, the
therapist asked the client to explore possible negative transference. Subsequently, the
client stopped canceling sessions.
Recent research supports the theoretical
assumption that insight alone does not bring about behavioral change. “What is
ultimately required is the forging of affective conviction to cognitive
insight” (Hoglend & Hagtvet, 2019, 8). But theorists vary as to which of the
“24 dimensions of emotions that can be conceptualized in terms of emotion
categories” (Cowen et al., 2019, 708) are most crucial to change.
Theorists also disagree about which of the
“27 distinct varieties of reported emotional experience” (Cowen et al., 2019,
700) are most common in therapy. Racker (1972) tells therapists to expect first
what is nearest to consciousness. Clients want to bond with their therapist and
therefore hope to be found worthy of their therapist’s efforts. Beneath this
hope, however, can be fear of being judged.5
Other theorists tell therapists to expect
feelings most likely to contribute to the therapeutic alliance, regardless of
their closeness to consciousness. On the positive side are feelings of love,
calm, and relief resultant from experiences of unconditional acceptance by
others being transferred to the therapist who, in turn, provides unconditional
positive regard. But even these feelings might be coupled with fear of
unconditional acceptance becoming conditional.
On the negative side are feelings of
distrust of a therapist who appears too good to be true, fear of being engulfed,
sadness because of previous broken promises, embarrassment, shame, or a
combination of these feelings. All can be transferred from experiences with
others.
Because bonding experiences are at least
partly negative, primitive negative feelings can easily combine with each other
and with positive feelings. In fact, the earliest bonding experiences commonly
consist of a positive experience of having one’s basic needs met on demand,
followed by a negative one of learning one has asked too much and/or too often.
To
decode feelings, then, is to derive the true meaning of complex and fluctuating
emotions that originally appear to be simple and stable. It is to study body language
along with “tune, rhythm, and timbre in speech because they are the truest
indication of emotions” (Bostanov & Kotchoubey, 2004). It is to listen
carefully to reports of dreams and fantasies and to consider the connotation of
words clients choose. Most importantly, it is to note whether there are
contradictions between or among various manifestations of transference.
She came late,
saying that she had rushed to get to her appointment. She was unsettled,
overwrought, and uneasy. When her therapist asked about her rushing, she simply
explained that she had not left the house in time. The therapist then had to
decide whether to take at face value a poor judgment of time and distance or to
decode her client’s words as possible manifestations of transference.
Noticing her
client’s uptight body and clipped sentences, the therapist decided to ask
directly about whether leaving the house late might be connected to reluctance
to come to her appointment. She then received what was a far truer answer. Her
client said that she was not sure that the therapist could really help her.
A fruitful
exploration of the exact nature of their work and the relationship it implied
followed, during which it became clear to the therapist that the client was
transferring her disappointment with former teachers to her therapist.
Feelings: Countertransferential
Even as therapists decode transferential
affect, they must be alert for countertransferential affect, for it can reveal
both the interpersonal weaknesses of clients and the work therapists themselves
must do to facilitate therapeutic progress. Having had negative experiences
with teenagers, for example, therapists can feel demeaned by adolescents. They
can perceive them as crass and self-centered, even moments after they enter the
therapy room. When adolescents sense this unspoken attitude, they can become
self-conscious. They can then come across as crass in their anxiety-ridden reaction to a person who dislikes them. Others have disliked them and inflicted harm, which has taught them a lesson: “Harm others before they harm you.”
Especially challenging for therapists are
countertransferential feelings transferred by clients who cannot tolerate, own,
or even put them into language because they precede their ability to speak
(Modell, 1980). Like infants who deliver subliminal affect-laden messages
before they can use language, clients unconsciously hand over their
feelings of being unloved, blamed, or confused to their therapists. Thus, by
unconscious design, the truth about clients is discoverable first in the countertransference
therapists experience when with them. Then it is discoverable in the transference
their clients experience when their therapists give evidence of their countertransference.
As a rule, therapists first
discover the truth about themselves in emotional reactions that are excessive
or inappropriate for what their clients are sharing (Tower, 1956). These
feelings are much nearer to the heart of the matter than reasoning. Indeed, therapists’
unconscious, affect-based perception of their clients is amazingly accurate. Moreover,
it is in advance of the conscious, cognition-based conception of the
interpersonal situation therapists form (Heimann, 1950). Emotions are
experienced far faster than thoughts are formulated, according to neuroscientific
research (LeDoux, 2002; Pally, 2002; Schaeffer, 2007).
As a
rule, therapists’ behavior or somatic response reveals their feelings.
Sleepiness, for example, can indicate that therapists have felt abandoned by
clients who frequently intellectualize, speak monotonously, or talk in circles
(Racker, 1972).
She moved from
topic to topic as skillfully as a skater circles a rink, returning periodically
to certain issues but never completely dealing with them. Her therapist grew
increasingly sleepy but tried to convince herself that a warm room and
insufficient sleep was making her head feel heavy. She wondered, however, why
nothing she did, including getting up to adjust the shades, alleviated her
distress. “Should I be decoding” the therapist wondered, “because the client is
‘saying’ more than meets the eye?”
Finally, the
therapist decided to test her hypothesis that the client’s circling speech
might be unconsciously intended to disconnect from her therapist. “When you
circle from topic to topic, I simply can’t stay with you,” she said. “I get so
frustrated that I disconnect from you. Could it be that you want to disconnect
from me?” she asked.
“I don’t know,”
the client responded, “but I do know that this happens to me a lot. I’ve been
so hurt by people not listening to me. Even as a child, when I said I wanted to
play with other children, they never heard me. I need help with how to talk.
I’ve needed it forever!”
Thus, decoding a countertransferential
response proved invaluable in terms of “unlocking” painful affect and exposing
childhood experiences from which the client continued to suffer.
Similarly, therapists’ feelings can
indicate enactments in which they have already become embroiled (Hinshelwood,
1999). Therapists’ irritability, for example, may be in the service of staving
off guilt feelings for having already acted out their dislike of a client
(Schafer, 1997).
We will now take a closer look at therapists’ countertransferential feelings, grouping those most commonly experienced (Cowen & Keltner, 2020). We will then look at the rarely discussed feeling of envy.
Countertransferential Sadness
Countertransferential sadness usually
combines feelings of worthlessness, hopelessness, helplessness, emptiness, depression,
and self-pity because of loss. Therapists’ depression, in particular, merits
special attention because it robs therapists of self-esteem and self-efficacy.6
Arlow (1985) claims that therapists’
depression is a countertransferential reaction: a defense against the
depression of clients. Clients come to therapy because of an unconscious sense
of a bad self even as they consciously proclaim a good self in relation to bad
others. Occasionally clients project a good self onto their therapist, but more
often it is a bad self (Epstein, 1977), which they subject to punitive measures
in unconscious imitation of prior caregivers (Racker, 1968). Therapists are
especially vulnerable to countertransference depression when treating
clients with Cluster B personality disorders (Betan
et al., 2005).
However, it must be acknowledged that
countertransferential depression also depends on therapists’ own sense of self.
Therapists with a positive sense of self and an internal “caregiver” are in a
favorable position to realize that their depressed clients are engaging in
projective fantasies which they must first resonate with, then soundly reject.
In contrast, therapists whose
self-definition is negative may unconsciously add self-punishment to negative
transference. Even worse, when therapists experience the combined force of
their inadequate internal self and their clients’ projections, they can lose their
capacity for rational, objective observation. They may never admit it to their
clients, but they “agree” intrapsychically that they are inadequate (Epstein,
1977), as the following vignette illustrates.
First the minister
came to therapy; then his son joined him. Their therapist, who had been
painfully humiliated by adolescent males, thought that in this instance she was secure. But
as the loose-lipped, surly adolescent attacked first his father and then other
members of his family, she had to admit that she was becoming increasingly
uptight. Soon afterward, the father appealed to the therapist to set limits but
still allow his son to express himself.
Feeling demeaned
when the son shifted his focus from people to the “stupid” therapy sessions
that he was being forced to attend, the therapist resorted to articulating what
she thought would be an acceptable agenda. People could express their feelings,
but feelings would have to be combined with discussion so that both father and
son could arrive at a solution they could both endorse.
In formulating the
plan, of course, the therapist was unconsciously attempting to lessen the
negative impact that the adolescent was having on her, even as she was
consciously steering the course of therapy from problem to solution. She was
determined not to succumb to the adolescent’s negativity. She would side with
the father in his need to get rid of it. She resolved that she would transform
the adolescent’s resentment into problem-solving energy and thereby reduce the
resentment she felt toward him.
Unfortunately,
this failure to address transference and countertransference issues proved
fatal. Imbibing his son’s attitude, as it were, the father began to align with
his son. He agreed that the family situation was so bad that it could not be
fixed and that therapy was a waste of time and money. The therapist was less skillful than she needed to be.
However, rather
than address her painful countertransferential feelings of inferiority and
impotence, the therapist again set out to convince the father, if not the son,
of the value of patience and hard work in therapy. She conveyed her hope that
things could change. As her own professional and psychological survival became
uppermost in her mind, she continued to act out – rather than decode – her
powerful countertransferential feelings.
Eventually, when
her agenda failed, the therapist admitted to herself that therapy was going
nowhere. She was incapable of reversing the negativity. She could no longer
count on her clinical expertise. When the father finally refused another
appointment, she merely mentioned her availability if he changed his mind.
Thus, the therapist’s insidious sense of
self-impotence and low self-esteem clouded her vision, which led her to
self-destructive despair. Her acting-in contributed to therapeutic
failure no less than did her own and her adolescent client’s acting-out.
Had she interpreted her depression to her clients, however, and asked whether
they, too, were experiencing painful feelings of inadequacy, victimization, and
resentment, it is likely that the father and son would have found her more like
them and thus more able to help them. They could have addressed the problem in
their therapy before, the problems they were dealing with outside of it.
Countertransferential Anger
As noted in the previous vignette,
countertransferential anger can include resentment toward abusive clients – if
not hatred of them – as well as disdain for victims of abuse combined
with revulsion and disgust for what happened to them. It manifests itself in
various forms of acting-out: withdrawing from clients (Plakun, 1998), becoming
irritable and restless because of precious time being taken up with what seem
relatively small problems, and even feeling bored or sleepy because of mundane
therapeutic issues. Countertransferential anger may also reveal itself as
therapists’ resentment of the emotional barrenness of clients’ communications
or helplessness and frustration (Cohen, 1952), all of which may induce
sleepiness.
Moreover, therapists’ extended frustration over lack of progress in therapy can produce countertransferential anger. This, in turn, can result in inattention, annoyance, and forgetfulness (Schwaber, 1990). Therapists treating clients with Cluster B personality disorders can be especially vulnerable to countertransferential anger (Bradley et al., 2005).
Countertransferential anger can also stem
from transferential guilt resulting from clients’ provoking their therapists
into acting angrily to appease their own guilt (Chused, 1992). On the
other hand, in response to aggressive transference, therapists may experience
subjugation and victimization. In time, however, even tolerant therapists feel angry
and vengeful (Racker, 1972). Then, if they try to relieve their distress
through subtle recrimination, they experience guilt.
At times, countertransferential anger can
also be provoked by clients’ rejection of a state of dependence that is being
“asked for” by therapists who assume the role of “savior” (Racker, 1972). At
other times, countertransferential anger can stem from therapists’ inability to
tolerate shame resulting from not living up to their clients,’ their
colleagues,’ and their own expectations (Winnicott, 1958). It can serve as a
defense against the experience of shame resultant from therapeutic failure
(Lewis, 1987).7
Ironically, countertransferential anger
can also be the result of therapists’ efforts to protect themselves
(Rothschild, 2000). It can be a response to having been threatened, hurt, or
scared.
Paradoxically, elevated anger, including
aggressive feelings, can be akin to a life force that can lead to
loving, hating, or both, as therapists continue to interact with their clients
(Winnicott, 1965). In turn, both hate and love can enliven therapists. They can
help them “to fix [themselves] in the world, to create a target for [their] own
feelings ….” (Becker, 1973, 144).
In sum, because anger is so intertwined
with other powerful emotions, it is a “given” in the course of therapeutic
work, regardless of therapists’ sincere desire to be benevolent. Ironically, countertransferential
anger can arise because of benevolent intentions.
Countertransferential Anxiety and Fear
Countertransferential anxiety, a response
to some internal stimulus (LeDoux, 1995), usually takes the form of therapists
feeling scattered and confused. They are unsure of relating to clients who
resemble others whom they have found difficult. They are uncertain of
therapeutic progress (Schafer, 1997).8
Countertransferential fear, in contrast, is a response to the environment. It makes therapists feel disconnected, disorganized, without control, feeling “like the floor [has been] taken out from under [them]” (Furlong, 2022, 20), and unable to think. This challenging condition tends to be a reaction to autistic clients (Gomberoff et al., 1990), attention deficit clients, hyperactive clients, or clients with Borderline Personality Disorders (Colli et al., 2014).
Countertransferential fear can also cause therapists to experience disequilibrium in response to schizophrenic or manic clients (Kantrowitz, 1997) or terror in the presence of clients with Antisocial Personality Disorders.
All of these experiences can result in
therapists’ desire to get relief by imposing their own ideas and solutions on
clients rather than patiently and painstakingly helping them discover at their
own pace what they must do to change.9
Therapists’ fear and anxiety can also
develop because they experience clients’ hold on them as an unconscious fear of
intimacy, seduction, engulfment, aggression, or dread of therapeutic regression
(Langs, 1979). Therapists may become apprehensive, for example, when clients
ask them for more time and attention than they can afford to give or feel comfortable giving.
Paradoxically, countertransferential
anxiety and fear may combine with guilt feelings and result in actions and
words indicative of submissiveness. This submissiveness, in turn, may cause
therapists to refer frustrating clients, to pamper those they do not refer, or
to search for quick resolution of complex situations to get relief
(Racker, 1972).
Countertransferential Gladness
Countertransferential gladness runs the
gamut from contentment to joy to elation. It may also manifest itself in
therapists’ feeling superior and wanting to boast (Handley, 1995) or to monopolize
the therapeutic conversation.
At times, countertransferential gladness
lures therapists into engaging in the unwholesome practice of competing with
their clients and their families or other professionals, such as medical
doctors or spiritual directors, in working with their clients. Therapists can
become insistent, for instance, that clients follow their advice rather than think
for themselves or consult others (Blum, 1986a).
However, the double-edged sword of
countertransferential gladness usually rekindles hope in clients and thus
proves extremely helpful. It contributes to the formation or repair of the
therapeutic alliance. But danger lurks even there, for gladness on the part of
therapists may induce in them positive feelings about therapeutic progress,
feelings that are unjustified because they rest on denial of still-needed,
difficult therapeutic work.
Countertransferential Envy
Because envy of clients is considered
shameful and unprofessional even when it is not acted out, therapists rarely
admit it. Unfortunately, however, therapists’ determination not to be outshined
by clients whom they envy at the same time that they help them is more common
than therapists would like to believe (West & Schain-West, 1997). Envy of
clients’ real accomplishments, or even of their potential to achieve, may lead
to therapists not supporting or encouraging their clients (West & Schain-West,
1997). Envy of clients may even result in premature termination if clients detect
therapists’ envy.
Identifying countertransferential envy
begins with becoming aware of the anxiety that accompanies it (Racker, 1968).
It includes being aware of the possibility of envy to morph into lack of joy
and satisfaction as therapists focus on their clients’ gifts rather than their
own.
Finally, envy might be operative if
therapists become verbose. They might be trying to prove they know more than
their clients.
Dreams
“There exists in us an internal stream of
intuitive knowing that is not in our conscious awareness. Paying attention to …
dreams lights a path, helping us know what we know and see what we see”
(Ferder, 2010, 86).
Dreams that clients bring into therapy are rich sources of
transference, especially if therapists are dream figures (Ferenczi, 1909). Therapists’ dreams are also valuable sources of countertransferential information if dream figures are clients (Tower, 1956). Jung, for one, found dreams he had about his clients to be crucial to his understanding of transference and countertransference, and to compensations he might be making because of poor attitudes toward some of them (Main, 2004).
Dreams are highly symbolic, containing
both primitive urges to act without regard to reality and rational motives for doing
so. They are often complicated, extended, and exceedingly confusing (Hedges,
2007). For they contain “clues about facets of [our] life that feel safe enough
to come out only in the stillness of the night” (Ferder, 2010, 86). Thus they are
worth extensive decoding.
Only an in-depth presentation would do
justice to the decoding of dreams, but the following vignette reveals the
value of doing so.
The therapist
noticed her client’s tight facial muscles and forced congeniality. She claimed
she was eager to work on assertiveness; but when her therapist began helping
her with specific assertive skills, she remained tense. It was only by decoding
her client’s dream that she learned what was really going on.
In the dream, the
client was being chased down narrow halls from one room to another. Wherever
she turned, doors opened into other rooms but never to the fresh, freeing
outside. The “enemy” chasing her was so close that she even felt its hot breath
down her back. The client thought that the narrow halls and rooms were those of
her own home. She thought that her critical, demanding husband was the “enemy”
always breathing down her back with his instructions. She couldn’t escape him.
She couldn’t get free.
While this interpretation may well have been accurate, the therapist
wondered about transferential implications. Could the rooms be the contents of
therapy sessions, which were packed with information but never let the learner
breathe freely and easily? Could the “enemy” chasing her be her therapist, whose
words felt like suffocating hot air? Could the client be feeling as if she were
being chased by a well-meaning therapist intent on doing good but nevertheless
robbing her of her freedom?
Sharing these
hypotheses, the therapist learned that her interpretation of the transference
was accurate. Had she not done this decoding, she would have never realized the
harm she was doing.
Fantasies and Daydreams
Fantasies are mental images created by
needs, wishes, or desires that occur during non-sleep states. Daydreams are
extended fantasies, even as fantasies are often “kernels” of daydreams. Though
both may seem simple, fantasies and daydreams are actually intricate, detailed,
and elaborate.
Fantasies and daydreams involve both
primitive urges and believable presentations (Herron & Rouslin, 1982). They
are means of accommodating to the environment, understanding what is occurring,
internalizing environmental events, and discharging energy from conflict
(Piaget, 1962). Hence, they can reveal transference and countertransference.
Furthermore, as fantasies and daydreams
bring ideals into reality, they become the basis for hopes and expectations in
interpersonal relationships. As ideals, however, they aid and abet
disappointment and dislike – even hatred – of real persons who inevitably fall
short of ideals. Yet fantasies and daydreams represent emotional “activity”
needing to be understood and worked on. They provide clues about clients’
emotional responses, including their reactions to their therapist (Herron &
Rouslin, 1982). Thus they call for decoding.
Unfortunately, clients seldom share
fantasies and daydreams with their therapists because they appear to be
distractions not worthy of attention. Consequently, therapists must be ever
alert to their presence, suspecting them in their own daydreams and fantasies
as well as in clients’ subtle movements and body language, particularly in
lapses of focused attention or mini-dissociative episodes. Clients whose eyes
become “glassy,” for instance, may well be daydreaming. Subsequently, they may
make reference to the heart of their reverie.10
One fruitful way of decoding fantasies and
daydreams is to look for the needs that they encode, particularly those that
can be met by others.
After a chance
encounter outside of the therapy office, the therapist found it difficult to
stop fantasizing about her client for several hours. “Strange,” she thought, “I
have so many other things going on.”
During
supervision, however, the therapist became increasingly aware of her positive
attraction to the client. His good looks, optimistic attitude, and refreshing
viewpoints made him “the perfect client.” “Still,” she asked, “why do I fantasize
about him?”
The therapist then
noticed subtle similarities between her junior high school crushes on
boys and therapy sessions with the client. She hypothesized that her positive
countertransference, related to her own need to enjoy those crushes, might well
be reflecting exactly what her client also needed to look at: the part he
played in sexual “rituals” that struck others as adolescent infatuation.
Indeed, her client had said that, though he disagreed, others said he was always flirting.
The therapist
worded her countertransference interpretation carefully during their next
session: “Could the thoughts I keep having about junior high days be
originating solely within me or are you contributing to them? They’re positive,
but would you say ‘out of place’ in our therapy sessions?”
The client was at
first bewildered. But when asked to take his time to respond, he realized his
attraction to his therapist, although he didn’t think that his feelings were
something that he could put into words. He never verbalized these kinds of
feelings, he admitted. He always tried to tell people that he liked them by
“just being himself.” “Could this be why people say I ‘flirt?’” he pondered.
Later, for the first time in his life, he dealt with behavior previously deemed
inconsequential.
Behavior
Manifestations of transference and
countertransference in behavior include body language, simple movement, complex
movement, and physical sensation. All are messages from unconscious to
unconscious through bodily means. “The body is the unconscious” (Pert, 1997, 141).
Indeed, “the basic units of experience are [not words but] bodily interactions
between self and others” (Fast, 1992, 449).
The behavior of the body contains key
information that determines exactly what clients and therapists are trying to
convey to each other (Scaer, 2005). Both are being
unconsciously influenced by a series of slight, even subliminal, signals.
Details of posture, gaze, tone of voice, and respiration are noticed and
recorded by both therapy participants (Meares, 2005).
Moreover, because the body cannot lie, it
is a source of truth about the present as it embodies memories of the past.11 The body has “the ability to tune in to the psyche: to listen to its subtle
voice, hear its silent music and search into its darkness of meaning” (Mathew,
1998, 185). Hence, in order to discover transferred material, therapists must
decode their own and their clients’ bodily behavior.12
Body Language/Simple Movement
Body language or simple movement refers to
inadvertent responses of the body to subtle, unconscious “messages” from the
right hemisphere. “You are in some kind of danger,” for example, is a common
message that makes clients fold their arms in front of them. However, when
asked, clients usually deny their fear, for the transaction that sent the
message from the brain to the arms was unconscious. Thus, it becomes extremely
important for therapists to study their clients’ and their own muscular
movements, postures, gestures, and other somatic reactions during therapy.
Of particular importance are right-hemisphere-controlled facial indicators, especially subtle movements around the eyes and mouth (Brownstein, 2007; Schore, 1994). For the left-hemisphere-controlled right side of the face, particularly the eye (Cowen et al., 2019), registers socially appropriate affective responses whereas the right-hemisphere-controlled left side, particularly the eye (Cowen & Keltner, 2020) divulges hidden personalized feelings (Mandal & Ambady, 2004).13
While what happens on a one-time basis may
not be worthy of much attention, body language that persists or repeats itself
is. For the unconscious mind produces again and again important material whose
overlooked messages need to break through to the conscious mind (Jung, 1946).
No matter what she
talked about, the client sat back in her chair, keeping a safe distance, as it
were, between herself and her therapist. “She has made progress, to be sure,
but could more be made?” her therapist wondered. “What needs to be done to
increase her comfort, if that is indeed a prerequisite for further work? Rather
than just space her sessions farther apart, I should address the sensitive
topic of our relationship and how it might be affecting her progress.”
During
the exploration that followed, the client reaffirmed her difficulty with
getting beyond the roles in which she had been cast as a child, roles so deeply
cultural that someone from outside her culture would hardly believe them. It
seemed as if the client needed to uncover the deterrents to changing her ways.
She had to trust someone who could understand how much she would be an exception
to her group if she changed.
“She sits back for
that reason,” her therapist decided, “She is telling me in body language how
alienated she feels.” So the therapist said, “It’s hard to trust someone from a
different culture, isn’t it? You and I might seem so different.”
To her therapist’s
relief, during the next session the client reported a shift in her attitude
toward making a change. She hadn’t made the change, she explained, but
she was planning it in detail. And she leaned forward when sharing her plan.14
Thus both therapist and client benefitted
from the close attention the therapist gave to transference and
countertransference being manifested in simple movements. Her noting her
client’s distancing, in particular, was crucial to her understanding her
client’s inability to trust a person from an often-abusive dominant culture
(Andersen & Przybylinski, 2012).
Complex Movement
In contrast to body language that encodes relatively simple messages, complex movement communicates several displaced feelings and story-like cognitions.
Complex movement occurs in both the mind and the body, according to recent research (Nardi et al., 2023). Thoughts and words become coercive actions loaded with emotion that usually relates to figures in the client’s or therapist’s early years. It is action dictated by a “script” never actually seen (Field, 1989), one most likely written between conception and eighteen months, when tone of voice, facial expressions, and gestures serve as primary means of communication (Meares, 2005).
Complex movement that puts transferred feelings and thoughts into action is usually called
enactment.15 It is the last step of “information processing that builds and exploits emotional databases of mind and brain” related to displaced material (Levin, 1997, 1136).
In carrying out transferential enactment,
clients assign to themselves and their therapist roles specific to past
experiences that have remained conflictual and thus carry heightened affect
(Schore, 2011). They “intend” to play a part and have their therapist play a
related one for various reasons, some of which might overlap.16 They are usually revisiting
the past in order to have it turn out better.
Alternately, clients may be unconsciously
testing with their therapist a pathogenic belief acquired in childhood
(Sampson, 1992), asking “Is that belief really true? Or will this person give
me reason to negate it?” Indeed, “during therapy, [clients] work according to
an unconscious plan to disconfirm their pathogenic beliefs by testing their
validity in the therapeutic relationship” (Gazzillo et al., 2019, 180).
Then, by closely monitoring their
therapist, clients hope for the evidence they need in order to substitute a
wholesome belief for one that is pathogenic (Silberschatz, 2005). The therapist
will have acted as “an implicit regulator of the [client’s] conscious and
dissociated unconscious affective states” (Schore, 2011, 84). “If therapists
pass their [clients’] tests, [clients] feel safer and frequently make progress
toward their healthy goals” (Gazzillo et al., 2019, 180).
Enactment of negative feelings and
thoughts is also called acting-out. Because it strains boundaries,
acting-out is considered a regressive interaction “experienced by either
[client or therapist] as a consequence of the behavior of the other”
(McLaughlin, 1990, 595). It must be quickly decoded and, if necessary,
examined, lest it limit the capacity for therapeutic work and exacerbate
extra-therapeutic interpersonal problems, for others soon find maddening the
“mind reading” required by someone acting-out. Clients must learn that others
greatly prefer words that describe feelings.
Meissner (1996) notes that “the potential
for countertransference difficulties to influence the therapist’s thoughts,
feelings, attitudes, and words is great enough. The potential for these unconscious
processes to find expression in the therapist’s … behavior and action is even
greater” (51).17
The same is true, of course, for
transferential difficulties influencing client’s behavior. In turn, on a
subliminal level, words used in therapy can become an incitement to action on
the part of both clients and therapists (McLaughlin, 1990). Both persons
unconsciously desire responses in themselves and others in line with their
transference and countertransference schema. Both want to “shape a happening,
bring about an enactment, in accord with [their] fears and hopes” (McLaughlin,
1990, 599). Both fear that the present might otherwise be simply a repetition
of the past. Both hope it will be improved, if not wholesome.
Countertransference enactment is often a
matter of therapists’ participating in the acting-out of clients’ transference.18 Therapists unconsciously collude with clients in mutual projective
identification organized primarily around clients’ unresolved conflicts
(Plakun, 1998). Thus, countertransference enactment conveys meaning regarding
clients’ transference conflicts (Sandler, 1976). Clients who are still
conflicted over wanting to be nurtured unconditionally and finding parental
figures unwilling to do so, for example, might fail to bring their copayment.
Should therapists refuse to play a parental role by asking instead for payment,
they will be actually addressing that conflict.
Countertransference enactment can also be
a matter of therapists’ own unresolved conflicts. Those with narcissistic
conflicts, for instance, might repeatedly insist that they are right (Wilson
& Weinstein, 1996). Those with aggressive conflicts might act belligerently.
Those with unresolved security conflicts might be dogmatic (Casement, 1991).
At other times, countertransference
enactment can be a matter of therapists attempting to counteract their own
weaknesses. Those who are indecisive, for instance, may exaggerate their
open-mindedness (Wilson & Weinstein, 1996).
An in-patient
adolescent ended his session by telling his therapist that another staff member
regarded her as incompetent. Unable to process her shame sufficiently, the
therapist set out to prove her competence. During a staffing two hours later,
she vigorously defended her client, blaming others for his bad behavior and
insisting on the soundness of her judgment. Unfortunately, exoneration was the
opposite of what her crafty client actually needed. He needed to take
responsibility for his behavior.
Impressed with the
therapist’s reasoning, however, the staff pardoned the client, who in time not
only repeated his misbehavior but took an even more adamant stand that he
should not be held responsible. He was the worse for his therapist’s erroneous
defense. He had been harmed by his therapist’s acting-out, a result of her
blindness to both his manipulating her and her own unresolved conflicts over
being thought incompetent.
Ogden (1994) thinks of countertransference
enactment as a powerful non-verbal “interpretation” being unconsciously
conveyed to clients. The “interpretation” may take a simple form, such as
ending a session early when stress levels are high. Similarly, instead of
asking for clarification, therapists may go off on a tangent when confused.19
Countertransference enactment has been
identified as an unconscious means of either indulging or punishing clients. By
indulging clients, therapists infantilize them: ask less of them than they are
capable of giving, provide for them what they themselves have the power to do
themselves, and absolve them of their obligation to change. By enacting rescuer
roles, therapists do clients the disfavor of not having them face their
dysfunctional patterns.
Therapists unwittingly indulge clients by “caressing”
them with words in order to quiet their own negative feelings. They speak in
soft tones or assure clients that all things are passing. They praise clients
for minor achievements that are more likely to be the result of chance than
hard work. Similarly, therapists try to divert clients from painful
countertransference-causing conflictual material by directing attention to
non-countertransferential material. By not addressing their own distress,
therapists spare their clients the pain of discovering their maltreatment of
others.
The therapist was
uneasy every time she met with her highly educated and wealthy client who had a
subtle habit of demeaning her. She did not want to admit this uneasiness,
however, either to herself or to him. Instead, she rationalized that she would
be noticeably prepared when her client came and thus prove herself his equal.
“Competition for outstanding performance is good for a person,” she said to
herself. “It makes people reach for the heights others have attained,” she
thought as she recalled seminars in which she felt inferior to male students.
Sessions appeared
to go relatively well as the therapist conveyed information the client
professed to want. On his termination form, however, he referred to a stifling
atmosphere in his sessions. There was an absence of free exchange, he wrote,
for his therapist seemed defensive. He couldn’t say that he felt disrespected,
but he knew deep down that mutual respect was simply not there. Rather, some
kind of a power struggle was going on.
Indeed, in a
primitive attempt to outdo one another, both therapist and client were
indulging each other on the surface but battling for superiority in the “deep.”
Sadly, by not addressing her countertransference, the therapist failed to help
her client deal with his dysfunctional interpersonal behaviors. In effect, she
punished him indirectly.
Punishing clients directly
includes discounting them. For instance, therapists can unconsciously perform
the exact opposite of roles clients’ assign. Plakun (1998) tells of a
previously victimized client assigning her therapist an abuser role. Instead of
exploring the client’s desire to be abused, however, the therapist spent the
time assuring the client that he was kind and caring. He would never abuse her.
In the course of doing that, of course, he was refusing to accept
countertransferential feelings of guilt. Thus he denied his client the
opportunity to work through her trauma related to being victimized.20
Alternative ways of punishing clients
include responding in a hostile, distant, frozen manner or taking a moralistic
stance that condemns clients. Therapists become excessively sympathetic to
third parties, for instance, and “take clients to court in a superior or angry
way” (Pick, 1985, 164). Alternately, they “forget” to bring up something
important, become highly distracted, or dissociate. Or they become silent,
whereby they strike a compromise between expressing their hostility and its rejection.21 They identify with a persecutor at the same time that they withdraw from that
identification (Racker, 1972).
In sum, whatever its unconscious
motivation, enactment is a psychic operation that is almost always related,
directly or indirectly, to the very reason clients enter into a therapeutic
relationship in the first place. It is also a psychic operation whereby
therapists unconsciously react to challenging aspects of their work with
clients. Dealing with it inappropriately mediates treatment failure (Plakun,
1998).
But dealing with it appropriately mediates treatment success, for it is usually the most authentic response therapists can make when unable to use words. It shows clients how they are affecting their therapist as well as those outside of therapy. It facilitates changing maladaptive relational habits (Shapira-Berman, 2022).
The client continued to think and act so narcissistically that her therapist was at his wit’s end. Verbal attempts to help her understand what she was contributing to her interpersonal difficulties had led nowhere. In fact, they motivated her to continue.
Finally, when his client rose to storm out of her session, her therapist also rose and spontaneously touched her client’s shoulders to stop her. Thwarted in her desire to leave, she yelled in protest. He said nothing for a few minutes, then spoke firmly but respectfully: “That’s enough. Be silent. Be quiet.”
At the end of their session, he was then able to say sincerely that he appreciated her cooperation and looked forward to their next session. His enactment had created a new reality, a new experience that became transformative as his client changed her overly self-focused habits.
Somatization
Yet another potential manifestation of transference is somatization: a source of truth known in the present but pertaining to the past. It is the body’s revelation of what happened earlier in the mind and “heart.”22 In fact, a growing body of research points to the importance of such phenomena
as intestinal flora and gut biome revealing one’s general sense of well-being
or lack thereof (Bach, 2019).
Similarly, recent neuroscience research reveals that experiences such as traumatization are recorded in the body on a cellular level (Van der Hart et al., 2006). Because of somatic changes in autonomic arousal, transference phenomena can be manifested in the body of a previously traumatized individual years after the trauma (Gene-Cos et al., 2016). An adult client’s smiling uneasily as she protests her love for her father, for instance, might be revealing negative experiences with him. For “implicit relational knowledge is not purely psychological but essentially psychobiological, mind and body” (Schore, 2011, 79).
Transference manifests itself in psychosomatic symptoms or illness aimed at drawing “the psyche from the mind to the original intimate association with the soma” (Winnicott, 1949, 254). Citizens of a country entered by immigrants, for example, can displace their concern about insecure national boundaries to their bodies in what is “roughly equivalent to the fear that [their] own body will be penetrated” (Lijtmaer, 2017, 692). Thus they experience heightened anxiety related to their belief that “racial minorities have the potential to ‘contaminate’ White Americans” (Tummala-Narra, 2019, 4).
Transference manifests itself in somatization because many unresolved conflicts occur in the pre-verbal period of life. Dealing with somatosensory information then becomes a major challenge to meaningful interpretation of its transference manifestations.
Somatization might be adaptive when it originally occurs, but it becomes maladaptive when ongoing because what is uncontrollable in early life usually becomes controllable due to development. It is adaptive to experience “butterflies” before being able to use language to manage anxiety, for example, but maladaptive to retain those physiological symptoms once reality testing reveals heightened anxiety is uncalled for.
Somatization in therapists, a twin of depression and a form of acting-in, is usually either a matter of thoughts stimulating emotions that then find bodily expression, or a matter of emotions themselves finding bodily expression. Like transferential somatization, countertransferential somatization manifests itself in symptoms and bodily conditions that have no physiological basis. Relatively common examples are sudden stabs of pain; tears; trembling; a growling stomach; strange sensations in the solar plexus; fits of coughing; poor sleep; sensitivity to noises; sleepiness, tightness, or tension, particularly in the chest (Chammas, 2023), throat, or jaw; nausea; rising heat; abdominal cramp; barely perceptible odors or tastes; and sexual arousal (Boyer, 1997).
“I am more than tired,” the therapist noted. “Most of my clients have been making progress. Why am I not relieved, even energized?”
It was only when some of her clients regressed significantly that she realized she was investing more energy in therapy than they were. One couple, for instance, became ambivalent about improving their relationship. Though they agreed they had to make personal changes, they resented having to make the effort. Furthermore, they revealed that they resented their therapist for saying so clearly that nothing else would save their marriage.
Being relatively sure of the countertransferential meaning of her fatigue, the therapist interpreted her countertransference in their next session. “I’m not sure why I am so tired after your sessions,” she said, “but could I be putting more into this work than you?”
“Now that you mention it,” the husband replied, “we are always being asked to account for what we did or did not do during the week. There’s more to life than doing therapy assignments!” After the conversation that followed, the couple finally began to take more responsibility for their progress. Slow but steady, their progress matched their own timetable rather than their therapist’s.
Indeed, it is crucial for therapists to stand in the spaces of different pieces of their self-experience and not use language too quickly, for words can never adequately substitute for bodily experience (Bromberg, 1991). Rather than telling clients what they think they know, therapists must listen to their clients and to themselves from an embodied place. To understand their clients’ displaced relational patterns, therapists must become aware of what they actually feel like in their own body (Looker, 1998).
In a fascinating article, Hedges (2007) gives a blow-by-blow description of how he used somatic countertransferential material when working with a client with a psychotic disorder, one who seemed extremely resistant to healing. After trying numerous other interventions, Hedges finally permitted himself to experience the client’s psychosis on a somatic level. “This is about me,” Hedges realized. “I have to let myself feel all of this” (23).
And he did. He then reported, “My mind swam in timeless … horror. I saw slaves being slaughtered and eaten alive by lions … tears welled up in my eyes. My stomach churned in violent upheaval. I stammered trying to speak what I was experiencing …. I had to rescue myself from the dizziness and emotional pull of the sadomasochistic pit …. I finally grasped at an experiential body level what [had] been perhaps [my client’s] deepest truth. … [My client] has for a lifetime feared relationships based on the template of a drugged and blinded cannibalistic scenario. He has experienced his emotional relationship with me according to the same pattern of abusive horrors” (Hedges, 2007, 23).
With this new countertransferential insight, Hedges (2007) was finally able to break the impasse he and his client had reached. “[My client] and I were together at last (23),” he wrote.
Damasio (1994) reminds therapists that somatization is common because emotions are actually conglomerates of sensations, which are integral experiences of the body. Each emotion has a different bodily expression, starting with a unique pattern of skeletal muscle contraction that is noticeable on the face and in body posture.
Each emotion also feels different on the inside of the body. Different visceral muscle contractions are discernible as body sensations that are automatically and involuntarily transmitted to the brain. Shame, for example, feels like heat rising in the face; sadness, like wet eyes (Rothschild, 2000).
Thus feeling of deadness in therapists might reveal how clients were neglected or loved and then rebuffed. Consequently, they never really experienced the vitality otherwise natural to infants (Field, 1989). Similarly, an inability to engage in deep breathing might reveal clients’ resistance to processing their emotions.
Hence, the next section is devoted to the important tasks therapists must perform in order to make transference and countertransference work for – not against – them and their clients
Diagnostic and Interpretive Tasks
In order to identify, decode, and
interpret transference and countertransference, therapists must involve their
non-verbal right brain as much as they do their verbal left brain. This is
because transference and countertransference, like most relational transactions,
rely heavily on client-therapist cueing and responding that occur too rapidly
for simultaneous verbal exchanges and conscious reflection (Lyons-Ruth, 2000).
The right brain, the repository of unconscious material, must assist the left
brain, the repository of conscious material.
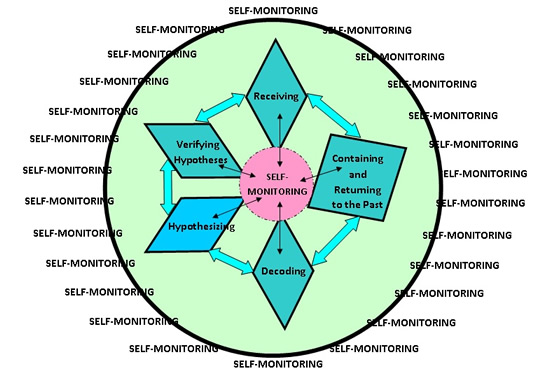
Besides using both hemispheres, therapists
must slow down their mental activity enough to perform five distinct but
interwoven tasks. All the while, they must monitor themselves closely in order
to decide how well they are performing each task and when they should move from
one to another. They must also integrate the tasks in order to accomplish their
main goal of interpreting transference and countertransference.
First Task: Taking In Transferred Material
Therapists perform the task of taking in
transferred material by making a conscious decision to continue to take in what
they suspect they have already taken in unconsciously, namely manifestations of
clients’ transference; and reacted to unconsciously, namely manifestations of
their own countertransference. This first task requires therapists to
deliberately open themselves up to what they sense they have already opened up to on an
unconscious level: conflictual contents of their own unconscious minds
attempting to enter their conscious minds.
Thus, the first task is a matter of
therapists trying to “be there” for clients and themselves in a new way (Heath,
1991). It is a matter of forming a composite picture of conscious and
unconscious information from which therapists and their clients can, in time,
derive authentic meaning.
The first task is fundamentally an acknowledgement of the nature of the human mind: it allows us to not only survive but also to thrive if—and only if--the conscious and unconscious minds work together. As Locke and Latham (2019) explain so well, the unconscious looks to the conscious mind for direction, but so does the conscious mind look to the unconscious for assistance as it struggles to navigate the real world. They can and do get each other “on board.”
Remember that the processes by which
therapists receive unconscious material from their clients and themselves,
namely transference and countertransference, operate first on an unconscious
level. Without knowing it, therapists receive the affective, cognitive, and
sensate messages their clients displace. Without intending it, therapists react
to subtle messages from the recesses of their own unconscious mind. At the same
time, they unconsciously transfer material to their clients.
When therapists perform the first task,
they intentionally “make room” for displaced material in their conscious minds.
They choose to increase their awareness of the feelings, attitudes, fantasies,
dreams, images, thoughts, sensations, and behaviors that they and their clients
are transferring (Bird, 1922). Therapists open themselves to a state of
“convergence” of past and present. They attend to their own unconscious
behavior as a possible sign of countertransference, asking whether they “are
playing an active role in one of [their client’s relationship] dyads” (Carsky
& Chardavoyne, 2017, 400). Thus they offer to clients their “entire
availability.” They give them all the time and mental space they need in order
to deal with their still-unresolved conflicts (Grinberg, 1997). In fact, the deliberate reception of transference begins a process whereby
therapists acquire the intuitive empathy necessary for the therapeutic
alliance.
In performing the first task, therapists
take seriously their professional responsibility to regard transferred material
as central to therapeutic reality (Deutsch, 1926). They become congruent with
the painful, unconscious memories of their clients (Vanaerschot, 1997).
By deliberately increasing their awareness
of what their clients are transferring, therapists also bring to consciousness
their own countertransference. They take note of the roles they are
unconsciously assigning clients as well as those their clients are
unconsciously assigning them. Therapists who are assigned a parental role for
clients working through early child-parent conflict, for example, deliberately
“accept” an image of themselves as a controlling, self-indulgent parent.
Similarly, if they themselves are assigning the role of unruly children to
their clients, therapists hold in focus the emotional satisfaction they have
begun to experience from subjecting a child to their will. They allow
themselves to note in detail the muscle tightness of one who is immobilizing
another, albeit in fantasy.
To
summarize, the first task is one of adding latent or suggested content to
manifest or obvious content. Therapists combine clients’ unconscious body
language and meta-language with what they consciously say. They also add their
own unconscious perceptions and desires to conceptions and intentions of which
they are already conscious, or which they at least suspect. Therapists allow
right-brain learning to augment left-brain learning. They open themselves to
receiving non-verbal communication that cannot be put into words.
Second Task: Holding and Permitting Regression
The second task requires therapists to
hold the transference and countertransference they have received, often for
more than one session (Bion, 1961). It also requires them to allow the
regression that tends to occur in a deepened and broadened holding environment.
The use of regression in this
context is an extension in meaning of a word originally reserved for an
unconscious process. Strictly speaking, unconscious regression cannot become
conscious. However, the process of willingly entering into a regressive state
so resembles doing so unconsciously that no better terminology has been found.
Regression
enables therapists to embrace the full impact of their clients’ displaced
reality. “This is the clear, sharpened, whole message my client is giving me,”
therapists come to realize as they hold various manifestations of transference
(Smith, 2000).
Therapists perform the second task by
containing and autoregulating their own negative states long enough to act as
affective regulators for their clients (Schore, 2003b).23 In turn, their clients become aware of their therapist’s successfully managing
the distressful feelings, sensations, and thoughts that they have transferred
to him or her. Benefitting from their therapist’s work, clients sense that they
can survive the anxiety that has kept these conflicts from reaching
consciousness. They can finally heal because their therapist is sharing their
“burdens.” As Wilkinson (2003) claims so rightfully, a safe
holding environment is the most potent vehicle for healing.
Casement (1991) describes this affect
regulation as therapists’ refusal to follow their natural inclination to
disengage from the distressful transferential communications their clients
send. They refuse to use words, for they tend to have the unintended result of preventing in-depth understanding from taking place (Miller, 2022, 24).
Rather, therapists avoid closure, tolerate ambiguity and uncertainty, subject
themselves to “total immersion to establish contact” (Bach, 2019, 6), and
permit lack of differentiation in order to share their clients’ displaced
relational experiences (Schore, 2003a). They do not return to their
clients prematurely what their clients project to them (Joseph, 1978). They
renounce their own need for gratification.
In performing the second task, therapists
refrain from taking refuge in words. They resist their impulse to shift into a
left-hemispheric dominant state and respond verbally to clients’ verbal
messages. Instead, they hold sensations evoked by unconscious communication
(Stark, 1994) and sustain the countertransferential feelings that transference
triggers. They stay in the right hemisphere, which has a “wait and see” mode of
processing (Federmeier & Kutas, 2002).
Thus, therapists do for clients what
clients were unable to do for themselves at the time of an original conflictual
experience. They allow psychic pain to remain in their conscious mind.24
As they remain open and mute, therapists
observe their clients’ posture, gestures, and movements, taking note of the
tone, syntax, and rhythm of their speech. Therapists allow their own felt sense
to act as a body-based perception of meaning (Bohart, 1993).25
For
the sake of understanding through experiencing, therapists permit
themselves to contain their clients’ unresolved conflicts in their own bodies
(Kernberg, 1987). They endure the disturbing thoughts, feelings, and sensations
their clients put into them.26 In more cases than not, they let clients use projective identification to
transform them into someone “bad,” someone deserving of disrespect, even abuse
(Gorney, 1979). They let themselves feel that unwanted label on a bodily level.
The second task also requires therapists
to re-experience the breadth and depth of their own unresolved conflicts,
phenomena that constitute a key element in any countertransference response
(Kernberg, 1975). Therapists willingly suffer the painful countertransferential
thoughts, affect, and sensations that reflect their clients’ conflicts (Roth,
2001). They deliberately entertain the countertransferential material that acts
as a stimulus for these conflicts to resurface.
Most therapists find the second task
difficult for three reasons. First, clients persist in displacing conflictual
material because on some deep unconscious level they are unwilling to entertain
the possibility of alternative perspectives. They want to hold on to the
illusion that they and their therapists are one person and that once their
therapists are feeling their pain, they themselves will no longer
suffer (Slochower, 1999).
On
the same unconscious level, therapists also want to hold on to the illusion
that they can resolve clients’ conflicts without holding the transference and
countertransference in which they are revealed. In particular, they want to
understand transference without experiencing it (Bonnet, 1991). They want to
make therapeutic progress in spite of distancing themselves from painful
displaced emotions. They want to do so by simply asking questions or shifting
their focus to routine observations (Schwaber, 1990). However, as clients take note of these false assumptions, they respond by
displacing their conflictual material yet again.27
The second reason therapists find this
task difficult is that they experience significant anxiety as they hold their
clients’ and their own displaced material, including the conflict-related roles
they have assigned and have been assigned. Clients’ toxic material mobilizes
therapists’ toxic material (Dosamantes, 1992). Therapists’ anxiety compounds
clients’ anxiety, which, in turn, exacerbates therapists’ anxiety.28
The third reason is that therapists
experience regression – to one degree or another – as they provide a holding
environment for their clients’ and their own primitive
cognitive-affective-sensate states (Winnicott, 1949). They regress “in the
service of countertransference” (Bigras, 1979, 312) as they contain their
clients’ distressful communication. They even risk experiencing disequilibrium
within their right brain that leads to deterioration in technical competence
(Spence et al., 1996).
In the middle of the last century, Little
(1951) described successful therapy as both a normal process of two conscious
minds sharing information and a pathological process of conscious regression. A
little later, Glover (1955) explained that therapy is fruitful because
therapists allow themselves to regress temporarily to early-life stages. They
permit themselves to enter a state of regression for the sake of broadening and
deepening within themselves their clients’ experiences.
Racker (1953) connects conscious,
intentional regression with therapists’ acceptance of the fact that although
they are adults and competent professionals, they are still children and
neurotic individuals. When therapists set aside some of the secondary aspects
of mature mental functioning and embrace primitive states, they feel neurotic.
When they deliberately allow themselves not only to hold but also to deepen the
hurt, anger, and fear inherent in the transferential roles their clients assign
them, therapists experience a strong urge to engage in retaliating, withdrawing,
or other counterprojective processes.
Rather than doing so, however, in
performing the second task therapists deliberately subject themselves to the
psychic forces that characterize transference and countertransference. They
relinquish the personal values and goals that are often rationalized and hidden
behind models of the mind (Schwaber, 1990). They intentionally allow disturbing
images, fantasies, and memories to arise: pieces of internal, unconscious
experience that are often contradictory, “crazy,” and disturbing (Isakower,
1963). They undergo fragmentary experiences that they hope will shed light on
or add clarity to perceptions of their senses and conceptions of their
conscious mind. Without a doubt, they perform some of the most complex clinical
skills one can acquire (Schore, 2011).
Therapists who are performing the second
task must use yet another demanding skill. They must not permit conscious
regression to impair their basic ego functions (Levin, 1997). In particular,
they must not lose hold of the fact that what their clients are transferring to
them still belongs to their clients (Deutsch, 1926).29They
must not become delusional and think, for instance, that they are in fact the
sibling of a client assigning them the role of an abusive brother. They must
not believe that they are allowed to actually perform their transferential
roles. They cannot initially prevent themselves from
receiving role assignments, but they must quickly get sufficient psychological
distance from those assignments (Ogden (1994). They must not own them, let
alone enact them. Instead, they must enable clients to own them and subject
them to reality testing.
In other words, therapists must not
suspend their ability to recognize and regulate the negative material being
projected into them. They must quickly identify it and use it in such a way
that their clients ultimately benefit from it.
Nor must therapists who are allowing
themselves to regress suspend their ability to recognize their own
countertransference and regulate its negative affect and disturbing sensations. In fact, in performing the second task, therapists must
dialogue with themselves often in order to balance affect and sensation with
thoughts about what is occurring and what needs to be done with it (Kernberg,
1987). They must periodically decide whether to begin decoding what they have
been holding or to continue to extend the holding environment for the sake of
getting additional information. Furthermore, they must ultimately decide
whether to process the displaced material they have received by working solely
by themselves, by consulting with others, by interpreting the material to
clients, or by combining these methods.
Said succinctly, because of the key
functions they must perform, therapists who permit conscious regression must
not allow themselves to go as far as to become thought-disordered.
However, therapists who regress may
experience a thought disturbance: things will appear false to their sense of
self. They and their client will feel as if the therapist were a parent. They
will accept, on a temporary basis, a parental definition that allows them to
want to act in parental ways.
In other words, when therapists permit
themselves to regress in the course of containing displaced material, they will
experience something that seems true on one level but false on another.
Regressing to babyhood at the request of a client who wants to be a parent, for
example, will seem strangely true from an affective standpoint but not true
from a cognitive standpoint. Similarly, regressing to the toddler age will seem
strangely true from a sensory standpoint but not true from a linguistic
standpoint.
When therapists temporarily set aside some
of the reality-testing functions of their ego as they entertain evidence of
past phenomena, they give their clients a powerful non-verbal “message.” They
say, in effect, that they trust their clients enough to become vulnerable in their
presence (Kantrowitz, 1997). They are allowing themselves to feel confused and
stupid at best, depleted and “lost” at worst (Money-Kyrle, 1956), and anxious
in any case (Wallerstein, 1990). They are choosing to remain in a “world"
where illusions and delusions are the norm.
Indeed, clients communicate early,
primitive material that is most important to them only when their
unconscious mind is fused with the unconscious mind of their therapist
(Isakower, 1963). Critical images, fantasies, and memories arise from both
client and therapist only when their minds are fused in a state of temporary
regression within the confines of therapy. Clients learn to observe the present
while experiencing the past only when their therapists learn to experience the
past while observing the present.
From the viewpoint of clients who have
regressed because of transference, nothing benefits them more than this. They
can trust one who has willingly descended into the depths of their painful
emotional state. They can trust a “kindred soul” who is also experiencing a
loss of understanding and insight (Bion, 1961). They can trust a “partner” who
is willing to learn their primitive “language” in spite of what it costs them.
With this basic trust established,
regression becomes for clients not only considerably less frightening, but also
enabling. It allows them to continue to convey a sense of early and complex
experiences otherwise not communicable. In addition, conscious regression
permits therapists to add key experiential data to information their clients
consciously provide, which, in turn, gives therapists a relatively complete
“message” they can decode.
Third Task: Decoding
Decoding, a left-brain activity, is a
matter of extracting the probable meaning of what clients and therapists are
displacing from the past to the therapeutic setting. It is a matter of deriving
hidden significance from apparent meaning. Decoding “breaks the code” in which
complex human communication is transmitted. It clarifies what therapists and
clients are attempting to share.
Decoding is a matter of discerning the
significance of garbled messages related to the work needing to be accomplished
in therapy. It is a matter of amending what is said in words by what is
communicated through body language, conveyed through association, or hidden in
symbols. Indeed, “wisdom is a return” to … symbols” (Jung, 1969a, 794). It
calls for decoding of those symbols.
Decoding is an essential task that therapists
must perform because truth and its bedrock of facts are usually shrouded from
both clients and therapists in spite of their earnest attempts to reveal them.
With rare exceptions, material that clients and therapists transfer from other
people to each other lies largely, if not completely, outside the awareness of
their conscious minds. Buried within the unconscious mind, it is inaccessible
to the conscious mind except in subtle, camouflaged signs.
Indeed, these encoded signs account for
impressions others receive without the senders intending to reveal themselves.
Not wanting to be known as hating their guests, for example, hosts make every
effort to show acceptance and tolerance. But when leaving, their guests may
hear a negative feeling word imbedded in such a superficially positive
statement as, “We hate to see you go.” In spite of themselves and the “front”
they have presented, their hosts have allowed their personal reality to “drip
from their pores,” as Shakespeare penned centuries ago.
Similarly, in the clinical setting, much
of what clients communicate is not really who they are and what they really
mean to convey. “[They] are who [they] aren’t,” wrote the poet Hafiz (c. 1350
CE) some 700 years ago. For clients have unconscious needs that are equally as
important to their well-being as solving their stated presenting problems. They
have both an anti-position in that they do not want to remain distressed
and a pro-position in that they prefer that distress to something worse (Ecker
& Hulley, 1996; Ecker, Ticic, & Hulley, 2012). They do and do not want
to resolve age-old conflicts with others. They do and do not want to be valued,
esteemed, and loved.
As a consequence, clients unconsciously
convey information that is quite different from their verbal explanations of
what they do and why they are in therapy. A client rushes in late, for example,
and blames his lateness on traffic. But because of subtle discomfort in her own
mind, his therapist suspects another message: “I am resentful.” She wonders
whether her client’s lateness is only the result of his battling
traffic. She wonders whether he resents something his therapist said the
previous session that made her resemble a disliked person in his past. In any
case, as the therapist questions the intent of her client’s explanation for
coming late, she inaugurates the decoding process.
Decoding is difficult for yet another
reason: therapists are unconsciously filtering reality through the lens of
their own experience and expectations. What therapists believe they perceive
may be different from what clients are actually communicating. The unconscious
message of clients cannot pass through the unconscious mind of their therapists
without some distortion.
Hence, therapists must also subject their
own countertransference feelings, attitudes, thoughts, and behavior to the
decoding process. For countertransference can be both informative and
misleading (Bach, 2019). What appears to be a positive urge such as wanting to
extend the session of the client who comes late, for example, might actually be
harmful because of its accompanying detrimental meta-message: “You are so
valuable that I will be uncustomarily generous with my own time. You do not
need to deal with why you are late.”
“Transference … has to be detected almost
without assistance and with only the slightest clues …” Freud (1905, 116)
explained a century ago. Since then, that task, and that of decoding
countertransference, have not become easier.
Thus, decoding is a multi-step process. It
entails deciphering mysteriously encoded psychological material. It requires
intensive cognitive work involving meticulous attention to detail. It involves
a willingness to evaluate vague intuitive possibilities and to struggle to make sense of what clients are really communicating (Miller, 2022).
In order to decode transference and
countertransference, therapists must first consider their clients’ and their
own choice of words, expressed affect, reported dreams, suspected fantasies,
and behavior, including somatic reactions. Some manifestations will be direct
contributions of the therapy participants; others, reactions to the
contributions that the other participant has made (Smith, 2000).
Then, therapists must hold in abeyance
apparent meaning while remaining open to interpersonal meanings beyond personal
meanings. They must take note of tone of voice, volume, word emphasis, gestures
that match content or fail to match it, and muscle movement that supports or
contradicts speech. They must consider nuances of human communication.
Therapists must also consider their own
feelings and whether they match those of their clients. They must acknowledge
bodily discomfort, noting sensations and physical responses that either
contradict or correspond to what clients are saying.
In
addition, therapists must be open to how they might be contributing to the
therapeutic experience of clients. They must be willing to distinguish what
their clients are inducing in them from what they themselves are bringing to
the therapeutic setting. Feelings of success during a session, for example, may
be explained more by occurrences removed from the therapeutic setting than by
the therapist’s skill and the client’s progress.30Similarly,
therapists’ feelings of envy may be due more to their own lack of similar
professional success than their client’s boastful demeanor. Of course, it may
be both.
“Why
does this client irritate me so?” the therapist queried. “Why am I not simply
flattered that he has come to see me? He is intelligent, articulate, and
seemingly ready and willing to get to the heart of his problems. Yet there
seems to be something subtly boastful about him. At least he strikes me that
way. Though he does so nonchalantly, he keeps drawing attention to the
recognition he has received for his research.”
In
pondering his own countertransference, the therapist suspected that he was
envious. He, too, desired to make a name for himself, but had not been very
successful. The difference between his own and his client’s professional
success was playing against his desire to be empathic, even neutral. He was
bringing to the sessions the pain of his disappointment with himself.
“Rather than interpret this
countertransference to my client,” he thought, “it would be good for me to
process my pain with a colleague.” If it continues in spite of that, I will
share what I am experiencing with my client. I will do so and ask him if the
effect he is having on me is unique to me.”
Fourth Task: Formulating Hypotheses
The process of formulating hypotheses
consists of therapists providing for themselves tentative explanations for why
the phenomena they have decoded are occurring. Hypotheses are probable reasons
why certain aspects of the past are re-occurring in the present.
Ideally, hypotheses are simple statements.
A hypothesis about familial relationships, for example, might be, “My client is
transferring to me her envy of her sibling.” The simpler the formulation, the
more clear-cut its verification can be.
In some cases, hypothesis formulation
occurs not after but at the same time as decoding. A therapist may think, for
example, that a client’s acting in an angry way, which includes giving evidence
of anxiety, is being caused by prior experiences of rejection. Thus, the
hypothesis at the time is likely to be, “My client is shouting at me because of
her anger and her anxiety related to her experiencing rejection from me.”
In other cases, hypothesis formulation
must follow decoding because the material is so complex that efforts to decode
it yield only an affective or cognitive label. The hypotheses that can be
derived at that time are limited to “My client is angry,” or “My client thinks
that I am mean.”
Hence, therapists formulating a truly
meaningful hypothesis must sometimes continue to look for causal links. They
must continue to open themselves up to the experience of their clients in
relation to themselves with the expectation that new and more specific material
will shed new light. The client who relates a story about a verbally abusive
bus driver encountered on the way to therapy, for example, may be unconsciously
providing an explanation of an original experience of victimization. But she
may also be saying that her therapist’s “taking” her down a certain therapeutic
road feels abusive to her. By continuing to listen carefully, her therapist
will receive confirmation of one, if not both, of her hypotheses. Alternately,
she may know that she must entertain yet others.
Fifth Task: Verifying Hypotheses
For effective therapy to proceed,
therapists must verify the hypotheses they have formulated. They may do so by
themselves, with consultants, and/or with clients.
One would presume that just as therapists
are eager to confirm their hypotheses, they are also eager to disconfirm them.
However, disconfirmation is significantly more difficult than confirmation, for
formulating hypotheses inaugurates a fondness for what is conjectured and
prompts a search for supportive evidence. Hence, to be effective, therapists
must learn the discipline of being as objective as possible about their
hypotheses.
A practical way therapists have of
accomplishing this is paying close attention to their own somatic response to
their hypotheses. The body will invariably, though perhaps subtly, “agree” or
“disagree” with what the mind concludes. Being physically energized, for
example, usually suggests appropriate hypothesis verification. Experiencing
repeated fatigue, uneasiness, or worry suggests the opposite. This is
especially true of hypotheses related to how helpful therapists are being to
their clients.
When her client
came in for his session, the therapist felt a deep calm. She was able to remain
appropriately focused on what he was saying and was usually able to resist
paraphrasing or giving advice when she needed to simply hold the material her
client was presenting. “He is given to intellectualizing,” she reminded herself
frequently. “He does not need me to offer additional intellectualization.”
Nevertheless, she hypothesized, “He is transferring to me an intellectualizing
function once performed by a significant other.”
On occasion,
however, the therapist did intellectualize instead of listen. She “grabbed” her
client’s thoughts and feelings and carried them swiftly to her mind, responding
cognitively. In no time, her body gave evidence of her interference. She lost
the calm she originally possessed. However, if she consciously returned to a
purely listening mode, she became calm and tranquil once again.
Thus, her bodily
reaction had verified her hypothesis: “He needs me to allow him to feel,” she
would henceforth remind herself. “He does not need me to help him
intellectualize.”
Supervisors and consultants are invaluable
during the verification process. In addition, especially in cases involving
significant countertransference, therapists may need to interpret transference
and countertransference to clients, asking them, in effect, to bring needed
clarity and accuracy to therapeutic material.
Indeed,
by interpreting transference and countertransference, therapists enable clients
to know experientially the benefits of identifying what actually is, rather
than to continue engaging in fantasizing. For only reality can serve as a solid
basis for changing what has brought clients to the therapeutic setting. Simply
wishing for that which is not merely prolongs immature psychological states and
reinforces negative interpersonal patterns.
Overarching Meta-Function: Self-Monitoring
Self-monitoring consists of internal
supervision for the sake of checking the quality of one’s work. It involves
three modes of operating: (1) watching in order to verify thinking, (2)
observing oneself in order to control affect, and (3) evaluating one’s behavior
in order to determine which actions to continue or discontinue.31
During therapy sessions, therapists
self-monitor for the sake of auto-regulating the stressful
countertransferential alterations that their client’s transferential
communications evoke. They attend to their own functioning even as they and
their client engage in mutual exploration of issues of which they are conscious
and communicate on an affective level (Perna, 1997). They maintain a “binocular
vision” (Holmes, 1992). They distinguish what they are feeling from what they
are responding to.
Self-monitoring during therapy begins with
therapists noting how well they are observing clients. For choices regarding
interventions that are intended to further the treatment plan must be made on
the basis of how they impact clients. Therapists must also note their own
well-being, for clients’ thriving is highly dependent on the therapeutic alliance,
which can be at least partially gauged by therapists’ sense of well-being.
By extension, therapists make calculated
observations of their interactions with the particular client with whom they
are working in order to judge whether their sense of self-efficacy is based on
those particular interactions rather than the client’s own innate capacity or
already-developed skills. “Is the direction I am going increasing my client’s
insight?” therapists ask themselves, “Or is she able to continue satisfactorily
without my interpretation?”
In one sense, therapists must self-monitor
continuously because of powerful forces such as transference and
countertransference that pervade the entire therapeutic process. It cannot be
emphasized enough that in the intimacy and regularity of the therapeutic
setting, reenactment of unfinished “business” takes place over and over again.
In another sense, however, therapists must
engage in self-monitoring periodically rather than continuously. Transference
and countertransference must have enough “room” to display themselves – even to
develop – during the therapeutic process but not so much “room” that they
enable full-blown acting-out or acting-in. If, through
transference, clients assign therapists the role of hateful parent, for
example, therapists must permit themselves to experience hatred of their
clients to the degree that its contributory “causes” become identifiable. But
they may not go so far as to say something hateful or let their neutral
statements carry hateful nuances.32
Similarly, if clients displace positive
feelings toward them – see them as a mother figure, for instance – at the
beginning of therapy, therapists must ordinarily allow the transference to
continue until the therapeutic alliance is firmly in place. But they may not
allow their clients to become dependent on them to the point of needing to call
regularly between sessions or finding themselves unable to provide honest
feedback when they feel patronized.
Thus, self-monitoring is especially
important during the first task. Therapists must consciously take in the
transference whereby they suspect both the roles they are being asked to play
and the ways they are inclined to play commensurate roles in the process of
countertransference (Hinshelwood, 1999). Therapists must also decide whether,
and to what extent, they might perform those roles as a means of furthering the
therapeutic and working alliances. Clients who are fearful of authority
figures, for example, might benefit from time-limited signs of maternal acceptance
or paternal approval.
Self-monitoring during the first task also
enables therapists to gauge to what extent they are unconsciously projecting
their own unresolved conflicts onto or into their clients. Without this
internal supervision, even experienced therapists are prone to simply re-enact
their clients’ maladaptive interpersonal experiences in countertransferential
behaviors (Dreher, et al., (2001). As a result, clients may never realize the
contributions they are making to their own unresolved conflicts and thus
determine how they might act differently (Weiss & Sampson, 1986).
Self-monitoring is also crucial during the
second task, when therapists contain transferred material and permit
regression. Therapists must stay with clients on a psychobiological level in
order to engage in necessary experiential learning, but they may not go so far
as to lose their ability to stand apart and take note of their participation in
transferential and countertransferential processes (Racker, 1972; Gorkin, 1996;
Gelso & Hayes, 1998). They must remain disengaged enough to ask a question like,
“How am I being manipulated to play the role of a demeaned person?”
Self-monitoring becomes especially
important when therapists permit conscious regression. They must become vulnerable
to the workings of displaced material at a sufficiently deep level, but it must
not be too deep (Winnicott, 1965). They must be partially aware of the process
they are undergoing in order to discontinue it at any time. They must
periodically employ their observing ego to “keep track of the pressure to
become trackless” (Schafer, 1997). They must “swim” in the sea of clients’
transference but not “drown” in their own countertransference (Racker, 1972).33
Furthermore, only if therapists monitor
their own regression can they be aware of the regression their clients are
undergoing. Because of non-analytic therapy’s customary time restrictions,
therapists must ordinarily stop their clients from full or severe regression.
But they can permit clients to engage in partial or mild-to-moderate regression
in the safety of the therapeutic environment. Most clients – as well as their
therapists – benefit greatly from carefully regulated exposure, in an interpersonal setting, to pain that originally so overwhelmed them that they could not process it on their own.
Self-monitoring remains necessary during
the third task, when therapists direct their attention to decoding transference
and countertransference, for these phenomena are operative even as therapists
are trying to derive meaning from them. Therapists must stand back to decode,
but they must remain available to their clients so that the length and
intensity of the decoding process do not seriously rupture the therapeutic
bond. Clients want to be accepted unconditionally, to be listened to intently,
and to be followed closely. They do not want their therapist to engage in the
difficult cognitive task of decoding for what seems to them too long. On
the other hand, therapists need to self-monitor to see if they are allowing
themselves enough time to decode accurately.
Self-monitoring during the fourth task,
hypotheses-forming, is necessary because therapists must decide whether they
are spending sufficient time and effort to hypothesize reasonably well. Though
they may not be sure of what is transpiring, they must come up with at least
probable explanations.
Self-monitoring continues to be crucial
during the fifth task, when therapists are verifying hypotheses. Therapists
clearly need to test hypotheses, but they also need to balance this cognitive
work with keeping an emotional connection with their clients. At the same time,
therapists must continue to receive and hold new material that will allow them
to revise inaccurate hypotheses.
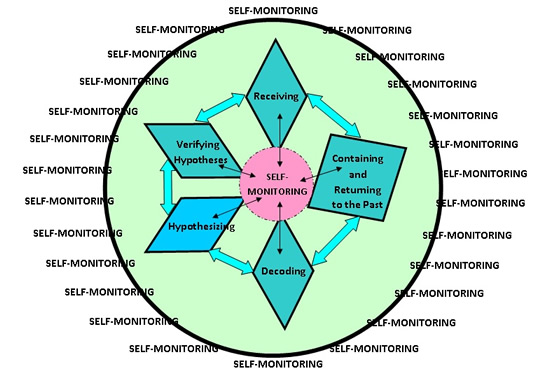
Finally, therapists must self-monitor
during all five tasks in order to be able to move quickly and smoothly from one
task to another. At times, therapists must decode what they have uncovered in
order to know what more they need to discover. Similarly, therapists may need
to experience more in order to verify what they think they understand. At other
times, they must gather new information in the light of their hypotheses
proving inaccurate. At still other times, when they suspect inaccuracy,
therapists must stop decoding and “test” their hypotheses.
Put simply, successful therapy relies
heavily on therapists’ self-monitoring their decisions related to focus: what
to focus on, whom to focus on, where to focus, and how to focus (Hubble, 1999).34
Wording Transference and Countertransference Interpretations
In order to appreciate specific guidelines
for wording transference and countertransference interpretations (TRIs and
CTRIs), we first need to define these interventions. We need to hold them up to
the light of the theoretical bases on which they depend as well as place them
within the context of non-analytic therapy. We also need to become familiar
with an attitude that has been found to precede and accompany effective TRIs
and CTRIs: openness to simply observing each client’s unique phenomenology and
one’s own distinctive reaction to it.
A Transference Interpretation
A transference interpretation (TRI) is a conscious and verbal phenomenon. It is intended to be an exchange between therapist and client that focuses on their relationship (Shapira-Berman, 2022).
A (TRI) is a
comment or question voiced by the therapist to call the client’s attention to
an apparent problem within the client-therapist relationship that appears to be
the result of transference. The therapist experiences a conflict between what
is transpiring in the therapeutic setting and the way the client and therapist
need to interact for their collaborative work to be fruitful.35
In the non-analytic tradition, a TRI may
simply state the transference-based problem, as in, “You seem frustrated with
me because of my limit-setting.” Alternately, the TRI may link the therapy
situation to a current or past conflictual relationship that the client has
described or alluded to (Pearson, 1995), a relationship that is being
transferred to the therapy session. The therapist may say, for example, “You
seem frustrated with me because I set limits the way your teachers did.”
A TRI that directly refers to displaced
material is “a creative re-description that implicitly has the structure of a
simile. It says ‘This is like that.’ It adds new actions to the life [clients]
have already lived” (Schafer, 1977, 57). It helps them see experiences before
therapy or outside of therapy as sources of unquestioned beliefs and
unchallenged emotions that are causing interpersonal problems. It suggests that
clients may be automatically imposing presuppositions on new experience
(Cooper, 1987).
The following TRI, for instance, would
help clients question their belief that all adults make unreasonable demands:
“I wonder if you see my request that you take care of your co-pay as the same
as your parents making you do your chores.”
Indeed, a TRI suggests that the
therapeutic relationship has become a re-enactment of clients’ previous or
current unresolved conflictual experiences outside of therapy. It is an
implicit acknowledgment of the powerful impact that people not actually in the
therapy room and events connected to them can exert on feelings and attitudes
arising in that room. It alludes to here-and-now cognition and emotion based on
there-and-then experience. It identifies clients’ unconscious expectations of
others. It asks them “to link their behavior to current relationship dyads in
the transference” (Carsky & Chardavoyne, 2017, 400) and evaluate its
appropriateness.
In other words, a TRI asks clients to
subject potentially harmful beliefs, emotions, and behavioral reactions to the
criterion of factual evidence. Clients may need to ask, for example, “I am
resentful, but are others’ requests actually unreasonable demands?”
Even a TRI that does not directly refer to
displaced material, but exposes a conflict in the client-therapist relationship
that has arisen because of transference, encourages clients to discover whether
their interpersonal schema are adaptive or maladaptive. “Are my expectations of
others realistic?” clients may need to ask.
Clients’ expectations tend to rest on both
conscious beliefs for which there is usually some objective evidence and
unconscious assumptions to which they have been holding fast, often against
objective evidence to the contrary. The belief that those in authority have the
power to make demands, for example, has objective validity. The assumption that
one person in authority will make unreasonable demands because another did so,
however, lacks objective validity. Nevertheless, in spite of unconscious
“certainties” never being personally validated, clients tend to accept them as
principles of knowing and guidelines for interpersonal relationships (Schafer,
1977). For example, clients experience their therapist as a person in authority
whose request for timely payment is unreasonable.
Consequently, clients need to look at how
they are unconsciously constructing the therapeutic relationship in accordance
with their unconscious principles of knowing. If they do not do so on their
own, therapists need to help them by interpreting the transference that betrays
the assumptions. “Could you be hearing my requirement that co-pays must be paid
as unreasonable as your being asked to get all A’s?” a therapist might ask.
Put in a slightly different light, a TRI
reminds clients that transferential wishes, feelings, cognitions, and
behavioral reactions connected with their present relational conflicts exist
within their own psyche and need to be recognized as such. They may or may not
reflect objective reality. Thus, a TRI is a means of performing one of therapists’
fundamental tasks: helping “clients recognize that current interpersonal
conflicts are, in actuality, intrapsychic conflicts” (Gill, 1982, 21).
Many TRIs also refer to the interpersonal
nature of clients’ conflicts. “I believe I have done something to anger you,” a
therapist might add, in order to recognize that the therapist is an active, though
unwitting, participant in transferential aspects of the therapy process
(Cooper, 1987).
Similarly, many TRIs clearly link previous
life experiences with emotions, cognitions, and behaviors arising in the
current therapist-client relationship (Cooper, 1987). “Could you be saying very little today because I angered you by being late, just as your mother was usually late when she picked you up from school?” a therapist might say. Other TRIs refer to current
experiences outside of therapy, as in “Could my going on vacation make you feel
abandoned, as did your best friend’s moving?”
Carsky and Chardavoyne (1917) support
Schafer’s (1975) theory of making therapeutic communication active by using verbs
and adverbs, rather than adjectives, in TRIs. Action language makes us realize
that all that happens in therapy is “some kind of activity …. An active verb
[states] its nature … an adverb, … [its] mode of action” (Shafer, (1976, 9) “Ways
of describing a person without making him the agent of action are problematic”
(Shafer, 1976, 11). They allow him to disclaim his actions while he carries out
the disclaimed action. Action language, by contrast, helps clients take
responsibility for their actions, change their problematic transferential
behaviors (Carsky & Chardavoyne, 2017), and make progress toward resolving
interpersonal conflicts.
Indeed, when therapists interpret
transference as a new here-and-now enactment of an old conflict and ask clients
to evaluative what they are doing, they bring to clients’ consciousness all
aspects of the new experience: its past origins, present operations, and future
implications. They invite clients to take a trip back in history for the sake
of insight (Cooper, 1987) regarding their unresolved interpersonal conflicts.
They invite clients to ask, “Should my behavior today be based solely on
long-held assumptions? Or should I see myself as an agent that can allow new
insights and facts to determine my behavior at this time?” (Carsky &
Chardavoyne, 2017).
Unlike a psychoanalytic TRI, which
suggests that clients process intrapsychically the information the
interpretation provides, a non-analytic TRI is an invitation to clients to
process the information interpersonally and collaboratively. A non-analytic TRI
encourages clients to talk about the dynamics of their session with their
therapist in order to arrive at insight in a relatively short time, as befits
session-limited treatment.
A non-analytic TRI is often a question such
as, “Could it be that you are angry with me because I sound like your mother?”
Though it may be a declarative statement such as, “I think you are angry with
me because I resemble your mother,” a non-analytic TRI still invites verbal
response because of its open-ended intonation.
There may be no clear, immediate agreement
or disagreement on the part of a client hearing a TRI. But generally, when
clients hear TRIs that strike them as accurate, they elaborate on the material.
When TRIs seem inaccurate, they do not.
Hence, Meissner (1996), agreeing with
Jacobson (1993) and Treurniet (1993), writes, “When the interpretive process is
working well, therapist and [client] are engaged in the exploration of
hypotheses [regarding their relationship] arrived at by a collaborative
process, based on the [client’s] intrapsychic content” (257).
At the beginning
of the session, the cognitive-behavioral-oriented therapist drew her client’s
attention to the fact that she had not paid her fee for the third week in a
row. Though the client acknowledged this and promised to write a check, she
responded curtly to several of her therapist’s subsequent reflections on her
accomplishments that week. Recalling the client’s stories about her overly
critical father, the therapist finally said, “Could it be that you are annoyed
with me today because I reminded you of your bill? Perhaps I sounded like your
father when he chastised you for not finishing homework.”
Responding to this
TRI, the client admitted that she was angry with her therapist. She refused to
admit, however, that she was displacing feelings toward her father, at least
not during that session and the one immediately following. In time, though, when
the therapist again made a tentative connection between the therapist’s
remarks, the client’s behavior, and their possible relationship with to her
father, she conceded. Afterward, the therapist and client were able to explore
together the deep pain the client had suffered – and was still suffering –
because of her father’s harshness.
Thus, by making conscious an unconscious
memory through an appropriately worded TRI, the therapist helped the client
free herself from having to remain a victim.
A Countertransference Interpretation
A countertransference interpretation
(CTRI) is a comment or question voiced by the therapist to call attention to a
problem that the therapist is experiencing which seems to be linked to
displaced material. The therapist shares that he or she is experiencing a
conflict between what is transpiring in the therapeutic setting and the way the
client and therapist need to interact in order to work well together.
At times, the CTRI links the feelings,
thoughts, and behaviors of the therapist to phenomena transferred to the
therapy session by the client. “I feel attacked by the remark you just made. I
wonder whether you are unconsciously trying to show me how your mother used to
attack you,” a therapist might say. At other times, the CTRI links the
therapist’s problem directly to his or her own displaced material. “I feel
demeaned by the comment you made, just as I sometimes felt demeaned by teachers.
Can we talk about what’s going on?” she may say.
At still other times, the CTRI suggests
that the therapist’s countertransferential response is linked both to the
client’s transferential behavior and to the therapist’s own personality,
history, or current extra-therapeutic life. “I wonder if my sleepiness is due
solely to not getting enough sleep or whether your silence in here is putting
me to sleep,” he may say.
In any case, a CTRI is an invitation to
clients to identify distortions, misinterpretations, and unfair attributions
that their therapist might be unconsciously making, with the hope that this
will increase clients’ insight into both their intrapsychic conflicts and their
interpersonal problems. However, a CTRI is not an invitation to explore the therapist’s problem as such. It is meant to facilitate an exploration of the client’s conflict.
As with non-analytic TRIs, a CTRI may name
only the therapists’ feelings, thoughts, and behaviors which the therapist
suspects are being elicited by the client’s transference. Especially when
previous CTRIs have done so, a CTRI does not have to refer directly to the
client’s transferred material. “I am frightened by your yelling when I ask you
to pay your bill,” for example, is a revelation of the therapist’s reaction to
a client’s reaction when reminded of similar events.
Similarly, a CTRI may simply refer to what
therapists themselves are doing in sessions. It may question whether
transference or countertransference is at work. “I feel so angry today and am
not sure why. Is something negative going on in here?” a therapist might say.
Though it does not do so explicitly, this kind of CTRI is still intended to
help clients identify what they are contributing to the client-therapist
interaction.
Finally, it is helpful to consider
Racker’s (1953) distinction between concordant and complementary CTRIs.
Concordant CTRIs tell clients that their therapist is identifying with them, as
in “I feel sad as I listen to you. I wonder if you are not both angry with your
spouse and sad about your marriage.” Thus the therapist is suggesting that the
client has transferred unacknowledged feelings to the therapist.
Complementary
CTRIs, on the other hand, tell clients that their therapist is identifying with
those affected by their client’s words and actions, as in “I feel humiliated
when I listen to how you deal with your son. Is it possible that your son feels
humiliated when you scold him?” Therapists are sharing their perception of what
significant others might feel when interacting with clients.
The client
elaborated on a pleasure trip he had just made, providing comical anecdotes
interspersed with interesting descriptions. Though she was at first intrigued and amused,
the Rogerian-oriented therapist soon noticed herself becoming bored and
irritated. The incongruity between his enthusiasm and her negative mood was
striking.
She began to
recall previously confronting her client about taking time off work in light of
his family obligations, for his goal was to have fun without neglecting
familial responsibilities. The therapist also wondered if her irritation might
also be due to her going out of her way to accommodate her client by rescheduling
his appointment for his convenience.
The therapist
hoped that by using a CTRI linking the client’s actions to her own irritation,
she could help him address an issue he had identified earlier. In the course of
that she might also process her own negative feelings, but that was not her
primary goal. She had noted her complex countertransference, but she would
focus only on an aspect of it clearly related to her client’s goal.
Eventually the
therapist interrupted the client and said, “I’m feeling irritated. Could it be
that your detailed account is preventing me from addressing how that trip might
have imposed a hardship on your family?”
Thus, the therapist used her own emotional
response to help her client examine his behavior and its impact on others.
The Right Attitude
Therapists who choose to share their
hypotheses about transference and countertransference with clients increase
their chances of being effective if they agree to simply observe and wonder.
“It is … observation itself, its meaning sought without preconception, which
enables the interpretation to follow in such subtle form that it may lie simply
in the answer given by the [client]” (Schwaber, 1990, 234-5). By
observing and wondering, therapists “say” to their client, “Let’s together
determine what is going on between us.”
“To observe and wonder is not to be ahead
of clients in ascertaining impersonal and personal reality. It is to give up an
agenda for understanding new and unique phenomena,” saying, in effect, “I know
less rather than more” (Schwaber, 1990, 237). When therapists simply observe
and wonder, they refrain from superimposing their preferred ways of thinking on
clients’ transferred material. They follow the lead of Winnicott (1960), who
said whimsically some 30 years earlier: “I interpret mainly to let the [client]
know the limits of my understanding” (711).
Therapists who simply observe and wonder
keep uppermost in mind that both transference and “countertransference [are
sources] of data but not [sources] of evidence” (Smith, 2000, 105). They
suggest complex realities but do not provide proof. Even if based on what
appears to be conclusive evidence, transference and, even more so,
countertransference are vulnerable to bias. Interpretations of them, conscious
derivatives of unconscious phenomena, cannot be used to describe them
definitively. Neither therapists nor clients are truly objective in spite of
sometimes feeling strongly that they are. Neither are without pathology,
anxiety, or vulnerability to defense mechanisms (Racker, 1972). Both are
holders of partial truth that can be known in its fullness only when parts are
put together.
Thus, therapists who wonder are open to
rejection or revision as much as to confirmation of their hypotheses. They
resist their tendencies to become attached to their interpretations and to
forget that they are only hypotheses (Cooper, 1993; Steiner, 1993). They await something
definitive – truth that develops only with the active cooperation of clients
(Bezoari et al., 1994) – rather than dispense to clients truths that they as
therapists have already gleaned (Cooper, 1993).
In fact, therapists who observe and wonder go one step further. They assign secondary importance to their knowledge in order to know clients by what they reveal (Smith, 2000). They create “a space for wonder, as opposed to reinforcing the well-trodden worldly response of shutting things down with exasperation [and] impatient shortness,” (Miller, 2022, 27).
They acknowledge the working primacy of the truth that the client holds and honor the fact that “everyone has a subjectivity worth knowing…. Every [client] is worth the fight,” (Miller, 2022, 27). For “it is the [client] and only the [client] who has the answers” (Winnicott, 1960, 711), however key to the client’s discovery the therapist’s intuition and insight might be.
Furthermore,
for therapists to observe and wonder is for them to simply watch the past
becoming dynamically present in therapy through transference and
countertransference. It is to understand gradually how the past is being
re-experienced in the present and to share that understanding with clients
(Casement, 1991). It is to be open to what might be the actuality behind the
appearance and the reality beneath the surface. It is to acknowledge that,
because material in the unconscious is highly undifferentiated, it is extremely
difficult to determine exactly what and how much clients, versus therapists,
are contributing. It is to wait and see whether countertransferential “truth”
actually resonates in the transference. For it takes the psyches of both client
and therapist to verify what is actually occurring.
Qualities of Effective TRIs and CTRIs
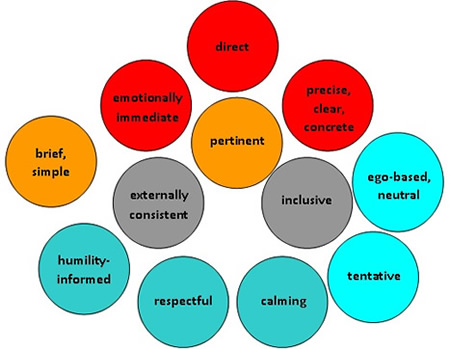
Effective transference and
countertransference interpretations are worded in such a way that they meet the
following criteria:
Calming
Though effective TRIs usually convey
disturbing information, they prove calming (Strachey, 1934) for three reasons.
First, they recognize the value of what might otherwise be considered
destructive subjective feeling states, as in “You seem to be angry with me. Can
we look at how that anger may be like your anger toward your spouse?” TRIs
indicate that, far from being unmanageable, emotions can be used to acquire
insight into a problematic interpersonal dynamic. TRIs allow painful reality to
finally overcome clients’ efforts to repress it. Thus TRIs bring relief, even
comfort, as they reveal what clients unconsciously “know” but prefer to deny in
spite of the immense psychic energy it takes to deny reality (Lear, 1993).
Second, because TRIs are voiced by
therapists who are noticeably calm, they signal that clients are in a safe
environment. Therapists are holding their own countertransferential response up
to the light of scrutiny without “falling apart,” collapsing, or retaliating
(Winnicott, 1960; Casement, 1991). When clients hear, for example, “By yelling
at me are you communicating your fury toward your…?” they can deny, confirm,
question, revise, or reject the TRI – all with impunity.
Third, effective TRIs reveal that
therapists have simply received a communication. They are not determined to
correct a client’s inappropriate behavior (Casement, 1991) or faulty thinking.
Clients can remain calm, for example, when therapists say, “In yelling at me, you
may be trying to show me what it was like to be your father’s son.”
Bollas (1987, 206) suggests that
therapists introduce TRIs with such calming phrases as:
- “I’m curious about
what you think.”
- “I’d like to share
a thought with you.”
- “You may not agree
with me, but …”
Beginning TRIs in such a way that clients
feel calm is the surest way that therapists have of not getting drawn into
client-initiated re-enactments. In the case of rage, in particular, therapists
can be unwittingly seduced into continuing an intense transferred feeling
through their TRIs.
In
order to make TRIs calming, therapists might also need to take a moment between
hearing and speaking during which they monitor for the potential re-enactment
concealed within the first interpretation that comes to mind. A short pause
between what clients and therapists say can serve as an indication that
therapists are truly “holding” what their clients are expressing. Therapists
are not so eager to process disturbing feelings that they cannot hold them
calmly as they begin an interpretative process.36
Like TRIs, CTRIs should calm both clients
and therapists. Therapists must even report feeling insulted in such a way that
they remain tranquil in spite of their unpleasant experience and the paranoid
anxiety that might accompany it (Little, 1951). They can survive being treated
badly (Winnicott, 1971) when transference is negative. Similarly, they can
manage positive transference, such as being idolized. They need not let it stop
them from demanding hard interpretive work of themselves.
Occasionally, therapists may need to
refrain from naming an emotion in order to remain calm. Instead of saying for
example, “I feel demeaned by your last remark and recall how you said your
mother demeaned you,” they might simply reflect upon what has just occurred.
They might simply say, “I am experiencing a communication from you that’s
coming in the only way you know – by behaving toward me as your mother behaved
toward you.” Having established a calm atmosphere, therapists can then use the
precise word for their experience without sacrificing tranquility.37
Similarly, therapists may need to preface
CTRIs by an explanatory remark in order to remain calm. “I get the impression
that you have often had the experience of being ‘the bad guy,’” a therapist
might say before adding, “I think that that’s why you put me in a similar
position and I feel blamed” (Casement, 1991, 147).
Of course, prosody must be equally calming
for TRIs and CTRIs to be effective. Therapists must convey calm through
secondary features like volume, tone, and pitch. In some cases, they must even
add a reassuring look or respectful gesture. This is especially true in the
case of clients with anxious/fearful disorders, for they tend to project
anxious/reoccupied transferences (Bradley et al., 2005). In other words,
therapists must convey to these clients that they “have a ‘soft spot’ in which
[clients’] affects can ‘hook’” (Gelso & Hayes, 2007, 28).
Emotionally Immediate
Strachey (1934) states emphatically that for
TRIs to be mutative, they must be charged with emotion. They must identify the
affect underlying clients’ transference conflict, however uncomfortable that
naming may be for both client and therapist. Furthermore, for TRIs to be
mutative, they must be given as closely as possible to clients’ emotional
experiences.38
It may seem contradictory for an
interpretation to be both calming and charged with emotion, but these qualities
are not actually mutually exclusive. Emotions can be expressed in varying
shades of intensity, all the way from hardly conveying the emotion to subsuming
content by loud volume and strident tonality. The challenge is to find a
balance between accurate reflection of emotions and their relative containment.
It helps if therapists think in terms of expressing their interpretations at
mild to moderate – rather than strong – levels of affect (Kiesler, 1982b).
Winnicott (1971) enjoins therapists to
examine and sift ideas and feelings that come to mind before they speak. Similarly, Ducharme (2017) advises therapists to take time to interpret transference and countertransference. After reflecting, for example, therapists can say, “You seem to hate me” in such a way that there is no doubt that the therapist has observed and recorded how the client feels about the therapist. But the therapist has not internalized the hate or necessarily found it justifiable.
Crowley (1988) uses an especially apt
metaphor to describe the challenge of balancing emotional immediacy with calm:
“It is tremendously important for [therapists] to burrow through the
exaggerated parts of [their] reactions to the healthy rational substratum ….”
(87). The anger that therapists experience, for example, may be largely
inappropriate, and they must recognize that. At the same time, they must use
the anger to hypothesize about what the client did to provoke it and why. They
can then meet the criteria of immediacy and calming. They can say, “You appear
to be angry with me right now because, like your father, I said that your pouting
is useless. Am I on target?”
Steiner (1993, 407) suggests beginning TRI’s and CTRI’s with such phrases as:
- “You feel better when I …”
Regarding countertransference, Maroda
(1995) suggests that therapists offer emotionally immediate CTRIs to
appropriate clients under most conditions. CTRIs are most effective not because
they are intellectual statements but because they are revelations of genuine
emotion. She says that “Ouch!” can be more effective than “I am hurt by your
remark!” Similarly, “I think your wife’s comment is very abusive. I can’t
believe that you didn’t get angry with her!” can be more effective than “I’m
disturbed by your not being angry with your wife.” However, Maroda (1995) also
warns that in formulating CTRIs, therapists must express feelings without losing
control. CTRIs, like TRIs, should be expressed at mild to moderate levels of
affect (Kiesler, 1982b).
Therapists
must also time emotionally immediate CTRIs carefully. Using them when clients
are already highly aroused can overwhelm them. Heightened anxiety, in
particular, can disrupt clients’ cognitive ability to profit from an
interpretation. On the other hand, therapists can help clients balance their emotionality with their ability to process their feelings cognitively by using a carefully worded CRI, such as “I’m concerned about your feeling I betrayed you. When you’re ready, could you tell me if that is the case?” In contrast, simply waiting until the client becomes less emotional can result in the client feeling betrayed because of the therapist’s not being honest (Bennett & Clark, 2021).
Ego-Based and Neutral
Volkan (1995) states that TRIs must come
“from the side of the ego,” (213) especially when clients are significantly
regressed. They must not come from the side of the id in that they simply
accept reality as it appears to be or one would like it to be, or to demand
that reality conform to one’s impulsive and instinctual desires. In contrast to
an id-based interpretation like “You are angry because I kept you waiting,” an
ego-based TRI would be “You may be angry because I kept you waiting.” The
wording of this second TRI implies that a strong reaction, while accurately
reflecting a client’s affect, is unlikely to be the totality of the client’s
state of mind and communication.39
Neither must TRIs come from the side of
the superego in that they pass irrefutable judgment on clients’ versions of
reality. Instead of teaching yet another version of the truth as understood by
the therapist, TRIs should be neutral with regard to the truth. The therapist might
say, “Your anger with me may be something that even you don’t feel good about”
instead of, “I think you are angry because you can’t tolerate the faults in you
that you see in me.” The ego-based TRI implies that no emotion is immoral in
and of itself. None are an unacceptable communication.40
Ego-based TRIs and CTRIs invite clients to
observe and face their own truth (Schwaber, 1990). They encourage clients to
examine what seems to be happening: to verify perceptions, check out
impressions, and elaborate on deductions. They further the client’s work of
reality-testing by facilitating a process within which a coherent truth can
gradually emerge. They are means whereby clients gain insights that make sense
of their transferential experience (Casement, 1991) and their therapists’
countertransference. An example of this would be “So even though you understand
… why I don’t call you when you’re anxious, you feel I am tormenting you” (Carsky
& Chardavoyne, 2017, 401).
In
some cases, TRIs and CTRIs are ego-based and neutral because they encourage
clients to process specific defenses being used by their ego, defenses that
should be dealt with prior to addressing primitive urges and impulses (Freud,
1926). Indeed, with many clients, therapeutic work needs to focus less on their
negative emotions than on the reasons they arise, that is, their defensive functions.41 An interpretation that identifies the insecurity underlying arrogance, for
instance, directs attention to where therapeutic work should be done. A TRI such
as “When you feel threatened, you try to protect yourself. Then I experience
you as being arrogant and overlook the possibility that you may be trying to
defend yourself from feeling small,” opens the door to an examination of the
defense rather than the emotion. It also undermines the combative atmosphere
created by the client’s arrogance.
The ego-based and neutral criterion leads
to an important corollary: it is often more helpful for therapists to use what
they “know” and find a way of approaching it through “not yet knowing” than it
is to simply reflect what clients are saying. An example would be, “You seem to
be envious of me as was your younger brother of you. But I sense you don’t want
to be.” Clients thereby get the message that their therapist is siding with a
reality-focused ego rather than a guilt-assigning superego. “I am afraid of you
today because of your shouting,” for example, simply reports the experience of
the therapist. This wording tells clients simply what therapists are feeling
and thinking about their clients. It counteracts a heightened emotional
response in them.
Similarly, a CTRI should not include a
justification for what the therapist is experiencing. “I am angry with you
today,” implies neither that the client is guilty nor that the therapist’s
feeling is justifiable. The emotion simply deserves to be looked at. It is to
be condemned by neither client nor therapist (Little, 1951). To make this
clear, therapists might add, “Can we take a look at what I am feeling and try
to understand it?” or “Would it be all right with you to explore where my anger
is coming from?”
Schafer (1983) says clearly that TRIs and
CTRIs are not to be unquestionable pronouncements or indisputable moral
judgments. Rather, they are to be expository communications as befits the
therapist’s clinical role. They are to be clarifying, explicating, or
enlightening observations. They are to come across as objective in that
therapists voice them without defensiveness, Gill (1982) adds. “You may be
angry with me” or “You appear to be angry with me” or “I believe you are angry
with me” are much less likely to carry condemnatory or judgmental overtones
than “You are angry with me.” Similarly, “I seem to be angry with you” or “I’m
finding it hard not be angry with you” are more ego-based than “I am angry with
you.”
Of course, the requirement to keep TRIs
and CTRIs ego-based and neutral also depends on tone, tenor, volume, speed,
pitch, and inflection, for the right prosody creates a respectful mood or
atmosphere. As Pick (1997) asserts quite accurately, some clients only listen
to the mood or atmosphere. They do not even hear the words. Hinshelwood (1999)
corroborates, observing that very disturbed clients acutely scan
interpretations to assess what their therapist is actually doing. They ask, “Is
he judging me? Is he retaliating? Has she forgiven me?”
In
sum, even a sensitively worded message will meet with resistance in a negative
atmosphere whereas a potentially painful-to-receive message will meet with
acceptance in a positive atmosphere. For clients tend to be acutely sensitive
to the hidden meaning in what their [therapist] says” (Casement, 1991, 131); to
the mood he or she is in.
Precise, Clear, Direct, and Concrete
Rather than being abstract or simply implying
that certain dynamics are occurring, effective TRIs and CTRIs are precise,
direct, and clear about the transferential distortions that clients or
therapists are making. They almost always contain the words I, you, and me (Bogwald et al, 1999). They name the specific actions that are
impacting therapy (Kiesler, 1982b). Effective TRIs and CTRIs give detailed and
specific information that clients can use (Strachey, 1934; Andersen &
Przybylinski, 2012). Clients can challenge the information upfront. Thus TRIs
and CTRIs befit the discerning role of the therapist (Schafer, 1983).
TRIs that clearly identify transferential
phenomena provide clients with precise information about how their behavior
contributes to interpersonal problems. They awaken unconscious resonances and
permeate intrapsychic boundaries (Lear, 1993). “You seem angry with me because
I said your eye-rolling is inappropriate, as did your teacher,” is clear,
concrete, and direct because it specifies the client’s behavior and identifies
an interpersonal problem. “You seem to dislike me now that I have suggested, as
did your mother, that you too are to be blamed,” and “It seems as if you are
afraid to tell me that you are angry with me. Instead, you just come late. Is
this true?” are also specific TRIs.
In contrast, if clients hear a TRI such
as, “Could it be that you are disturbed because of my remark?” or “You seem to
be getting upset about what I’m saying,” they may be unsure about what “my
remark” or “what I’m saying” means. Vague, imprecise TRIs can also give clients
a chance to thwart their therapist’s attempts to bring unpleasant unconscious
material to consciousness (Strachey, 1934). Similarly, clients may not give
them much attention or even hear them (Bogwald, 1999). Indeed, the unconsciousness looks to and depends on the conscious mind for direction. At the same time, the unconscious can get the conscious mind “on board” (Locke & Latham, 2019).
Like TRIs, CTRIs should bear
correspondence to historical facts or to specific features of clients’ scripts
(Joyce & Piper, 1993). Ideally, CTRIs should refer to clients’ presenting
problems, major themes in their goals, and the metaphors they repeatedly use.
“I’m frustrated right now because of not getting any helpful information today.
Does your spouse also get frustrated when you don’t share with her?” would be
an example.
Ideally,
CTRIs should include clear, direct references to what is happening in therapy
in the here-and-now. They should identify specific affective reactions that
therapists have experienced or concrete behaviors they have performed. At the
least, CTRIs should identify events that clients will recall as having occurred
in the therapeutic setting (Strachey, 1934; Swift & Wonderlich, 1990;
Stolorow, 1993; Stone, 1984; Strupp, 1989; Casement, 1991; Piper et al., 1993).
A therapist might say, for instance, “I looked at my watch so often
today. Perhaps I want to disconnect from you.”
Tentative
At first it might seem as if the criteria
of clarity, precision, directness, and concreteness on one hand, and
tentativeness on the other, are mutually exclusive. But both criteria can and
do apply. Effective TRIs and CTRIs should convey specific information as well
as indicate that they can be explored, revised, even rejected (Steiner, 1993, 421). They are not conclusions drawn by therapists. They are invitations to clients to collaborate in
discerning the validity or invalidity of therapists’ observations. They
are “meant to be played with, kicked around, mulled over, and torn to pieces
rather than regarded as official versions of the truth” (Bollas, 1983, 7).
If interpretations are tentative, they make it possible for clients and therapists to gain in-depth understanding of the client’s world as well as how the therapist’s mind is evolving. They move phenomena “from being viscerally felt into something that can be understood in a new way,” (Miller, 2022, 28). They give clients who “may have never found someone who was actually curious about what they had in mind” a chance to heal from having “learned that their own minds are unwelcome and must give way to how others feel a situation should be thought about and interpreted,” (24).
Contrastingly, if therapists are always certain of what
they say, clients have to contend with a dogmatic individual who claims to know
more than what is actually knowable (Field, 1989). Many clients feel pressured
to submit to a purely receptive and acquiescent style of working (Bacal, 1990).
They do not feel free to interact with their therapist in an effort to find out
which of several potential meanings is the most accurate (Winnicott, 1971).
In other words, when therapists honor the
criterion of tentativeness, they introduce a subjective state of mind: they
offer to their clients “a scrap of material and a chance to elaborate on it”
(Bollas, 1987, 206). They indicate that they are open to questioning,
clarification, and revision. They, too, might be uncertain at the time transference and countertransference are unfolding (Bennett & Clark, 2021). They are listening for evidence or consensual
reality that supports their own or their clients’ perceptions and judgments
(Schafer, 1983). They are hoping that both they and their clients can correctly
identify their displaced perceptions and feelings.
Therapists can indicate that their TRIs
and CTRIs are tentative by prefacing them with such phrases as:
- “Perhaps it’s that
I don’t know whether you will agree with me, but …”
- “I don’t know if
you are going to like what occurs to me, but …”
These prefaces make the TRIs and CTRIs
that follow more communicative than informative (Brodbeck, 1995) though they
offer information. They are more probabilistic than certain (Schafer, 1983)
though they are precise and concrete. They clearly invite clients
to respond in agreement, disagreement, or partial agreement (Bollas, 1987).
It is especially important, Bollas (1987)
contends, for therapists to acknowledge the difficulty of putting into words
what they believe clients are feeling toward them. When therapists
struggle to find the right words for what their clients experience, they model
how to deal with what they somehow “know” but cannot clearly describe, or with
what they suspect but may never have known. Therapists counteract that
certainty with which clients have often been judged and judge themselves. Instead, they
invite clients to join them in an effort to discover the complexities of the
human person and interpersonal relationships.
Indeed, by using tentative TRIs and CTRIs,
therapists underscore the wisdom of passing subjective perceptions back and
forth until only those that withstand scrutiny survive. By using tentative
rather than irrefutable TRIs and CTRIs, therapists make a fundamental
distinction between interpreting “countertransference as one indicator
of what might be going on in a complex field and using it as the complete explanation of what is transpiring” (Herron & Rouslin (1982, 146) [Italics
mine].
Tentative
phraseology is even more appropriate for the countertransferential “unthought
known”: what therapists feel but do not understand because material is being
transferred from extremely primitive parts of the client’s unconscious mind
(Bollas, 1987, 232). Yet this material is extremely valuable because both
therapist and client intuitively recognize it as meaningful though the core of
its significance has yet to be discovered. “Could it be that my frustration
today is related to some kind of message you are giving me? I can’t put my
finger on what is causing this feeling,” the therapist might say. This wording
is likely to reduce defensiveness, which is especially necessary in the case of
clients with dramatic or eccentric personality disorders, for their transferences
tend to be angry or entitled, even sexualized (Bradley et al., 2005).42 They and their therapist can then “play with” meaning and significance in a
relaxed and respectful way (Winnicott, 1965), kicking them back and forth until
meaning becomes lucid and significance compelling.43
Pertinent
Effective TRIs and CTRIs are also
pertinent in that they refer to client’s concerns and issues. They lead to
insight that is specific and often quite new (Casement, 1991). They are
intended to enable clients to attain their goals.
TRIs and CTRIs are especially pertinent if
they refer to problematic core conflicts occurring in the present both outside
and within the therapeutic setting. By interpreting the here-and-now,
therapists bring hope: the past cannot be changed, but the present can.
To meet the criterion of pertinence a therapist might say, for example, “Have you not identified so long and closely with your father’s poor opinion of you that you can no longer be you?” (Evans, 2022).
TRIs and CTRIs referring to the
client-therapist relationship as it evolves are particularly useful. They zero
in on “unresolved impediments to congruous and continuous relationships with
people in the present” (Wolstein, 1996, 505), both the therapist and people
outside therapy. They shed light on both intrapsychic and interpersonal
challenges to goal attainment. For most personal problems arise from unresolved
interpersonal conflict (Wolstein, 1996).
The criterion of pertinence is based on the fact that it is often very
difficult to discern the true source of clients’ and therapists’ feelings
toward each other, although both parties perceive subtle feelings.
Many pertinent TRIs and
CTRIs simply identify feelings, for most often feelings precede thoughts. If
correctly identified, they can lead to thoughts about why they are arising and
what can be done about them. For the past lives on in the present in the form
of sudden, strong, or unusual affective and somatic reactions in therapy
sessions.
However, the criterion of pertinence does
not require therapists to tie “then” and “there” happenings to “here” and “now”
incidents. If they are actually linked, clients will link them, mentally if not
verbally. Or therapists themselves will obtain further data to link then-and-there
phenomena to here-and-now phenomena in subsequent interpretations.
Inclusive
Though the criterion of pertinence allows TRIs
and CTRIs to refer only to the present, there is a place for inclusive
interpretations that explicitly link the present with the past, or
therapeutic interaction with that which occurs outside of sessions. When it is
relatively clear that therapeutic events are being triggered by non-therapeutic
experience, therapists may say, for example, “I wonder if my being judgmental
toward you today is partly due to your having found reasons not to come to sessions
for several months.” Or they may ask, “Is my being judgmental toward you today
solely the result of my headache?”44
In some circumstances, if TRIs and CTRIs
are not inclusive, clients may feel more comfortable but draw erroneous
conclusions. Simple here-and-now TRIs and CTRIs may imply that therapists are
afraid of their feelings. As a consequence, clients may suppress their strong
feelings for fear of their therapists not being able to cope with them.
Similarly, here-and-now TRIs and CTRIs may lead clients to think that their
therapists’ examination of the therapeutic relationship is being done at the
expense of their presenting problems (Bauer & Mills, 1989).
One way to meet the criterion of inclusivity is to start with an observation that the client has made about the past and follow the direction of the transference to where the past is spilling over into the present. For example, “When you were dependent upon your mother, she left you. Because you were feeling dependent on me before I took a vacation, are you now experiencing me as the mother who went away?” By wording TRIs this way, therapists are offering insight into the client’s past distress while keeping the focus on the present. They are helping clients recognize that they have projected early life figures on their therapist and expect them to behave the same way (Steiner, 1993).
Similarly,
clients can benefit from therapists’ introducing material from a previous
session while focusing on the session at hand. “Last week you spoke of John,
who abuses you. I wonder if today you are finding me abusive,” for example. In
fact, Gill (1982) recommends routinely including also or in addition as a way of making TRIs and CTRIs inclusive. For these words clearly link
“there” with “here” and “then” with “now.” Thus clients are “helped to learn
the ancient and deep source of the re-experienced impulses. As a result,
remembering and re-experiencing become organically blended” (Kahn, 1997, 59).45
Brief and Simple
Making TRIs and CTRIs inclusive, however, does not remove the criteria of being brief and simple. They should not require such extensive cognitive work that clients and therapists have to push down their feelings for very long. For suppressed feelings tend to become very distressful.
Matte Blanco (1975) rightly argues that TRIs and CTRIs should be simple because transference and countertransference, products of the unconscious mind, are relatively simple. The unconscious considers only one characteristic of objects, disregards all others, and makes one feature equal to the whole. While this process is certainly not simple in the strict sense, it bears the stamp of deduction and reduction and consequently puts the client’s mind in a simple mode. It makes the client comfortable with interpretations in that same mode.
Harry Stack Sullivan (1954) purportedly said that interpretations should be no longer than seven words (Swift & Wonderlich, 1990). Others disagree. Though they may be more than seven words, they should be short (Strupp, 1989), simple (Schafer, 1983), and to the point (Joyce & Piper, 1993).
Thus for the sake of brevity, therapists might have to divide a complex TRI or CTRI into two successive TRIs and CTRIs, with the first addressing just the emotional or cognitive-emotional nature of the client-therapist relationship and the second adding the extra-therapeutic or pre-therapeutic aspect (Roth, 2001). For example, after saying, “I wonder if you are turning me off because I have hurt you,” a therapist could add, “It could be that you feel hurt when your wife fails to appreciate your help, as you mentioned earlier.” Or after saying, “Could it be that you [come] late to express contempt for my efforts to help you … ?” a therapist could add, “And at the same time this deprives you of my help, as if you see yourself as the one who is not worth the time” (Carsky & Chardavoyne, 2017, 400).
A second way to ensure brevity is to focus
on just one aspect of the transference: how clients’ experience of the
therapist relates to schemas clients hold (Gelso & Hayes, 1998). Therapists
might simply say, “It seems you can’t trust me because your sister betrayed
you. You use what she did to you as a model of how other women will act.”
Alternatively,
therapists might focus on just one feeling or one behavior. “I am impatient
today,” is preferable to, “Even though I want to be patient today, I am feeling
impatient.” So is, “Your not coming on time frustrates me,” preferable to,
“Your not coming on time and presenting a hard-to-believe excuse frustrates
me.”
Respectful
Respectful TRIs and CTRIs leave clients
feeling recognized, acknowledged (Shapira-Berman, 2022), accepted, affirmed, and esteemed even though they have developed
dysfunctional relationship patterns. Far from feeling demeaned, clients feel
respected for their approach to life and their struggle to change (Kiesler,
1982b). Far from feeling attacked in isolation, clients feel included as
collaborators in a process designed to help them earn respect.
Respect is not easy, however, when clients
express pronounced, pervasive negative transference and are resistant to
looking at it. It is hard for therapists to refrain from bullying them, most
often through an attacking style of interpreting what is rationalized as “dealing
with resistance.”
To counteract this and make sure that TRIs
and CTRIs are respectful, therapists are wise to remind themselves that
pathology is not only a defense but also a form of communication without which
some clients cannot get along (Casement, 1991). “It seems hard for you not to
be angry with me,” a therapist might say. “You seem intent on helping me know
how awful someone’s anger can feel," she might add. She would thereby remind
both herself and her client that harsh treatment of others is more often
intended to communicate distress than punish others.
Recent neurocognitive research also
suggests an approach that clearly recognizes the conflict being held in the
client’s mind. On a conscious level, the client wants to change; on an
unconscious level, the client does not want to change because that might mean
something worse than what is being suffered. Ecker and colleagues (1996; 2012),
for example, recommend that therapists bring that contradiction to light by
saying something like, “Part of you wants to stay depressed and part of you
wants to get rid of depression.” Thus a TRI might sound like, “Part of you
wants to work with me to get rid of your depression. Another part of you wants
to write me off and stay depressed.” Clients are then confronted directly with
a contradiction but still feel respected. Their therapist acknowledges a
maladaptive but understandable reason for their resistance.46
Humility-Informed
Making TRIs and CTRIs humility-informed is
related to making them ego-based. Truly humble therapists who share their
interpretations do not imply that they are superior to their clients in insight
or intelligence (Bollas, 1983). They accept, rather than deny, their weaknesses
and limitations. They are skeptical about their own objectivity and how well
they perceive their clients’ reality (Gill, 1982).47 They offer equal partnership in a process that creates or “restores
mutuality in the ‘affective response’ of one to the other” (Winnicott, 1960,
117).
Therapists using humility-informed TRIs and CTRIs are taking at least partial responsibility for what is happening in therapy (Ducharme, 2017). They usually begin their TRIs and CTRIs with such humility-informed phrases as,
- “This may sound
crazy, but …”
- “I could be way
off base, but …”
- “I don’t pretend
to know more than you, but …”
By starting out this way, they enable clients to feel secure. They can survive revealing – and hearing their therapist reveal – their personal weaknesses because their therapist also acknowledges limitations and wants to learn from mistakes (Casement, 1991).
The humility-informed criterion also calls for therapists to be wary of minimizing their countertransferential reactions. As a general rule, they must not deny the truth; they must not tell themselves that the distress that they are experiencing is too insignificant to mention. Racker (1953) warns against failing to interpret countertransference because it does not seem worthy of attention. Even more important, therapists must not refrain from using a CTRI to avoid feeling humbled. An example of such well-worded CTRI is “I’m concerned that I’m coming across as giving up on you. Is that the case?” (Evans, 2022).
Externally Consistent
Finally, TRIs and CTRIs must be externally
consistent: sensitively timed and accompanied by appropriate tone, volume, gestures, and
other meta-verbal characteristics. During the course of therapy, however, as
therapists are eager to accomplish goals, they may use TRIs and CTRIs too soon,
too frequently, or too enthusiastically. Just as moderation is always the best
rule, so is careful monitoring of clients’ level of anxiety or comfort. So is
careful monitoring of therapists’ own tendency to use TRIs and CTRIs simply to
express negativity or to accomplish their own goals rather than patiently
seek the well-being of their clients.
It
is Blum (1986b) who warns therapists most succinctly. “Even where
interpretation is correct in content, the countertransference [or transference]
may be conveyed through inappropriate timing, tact, or tone, and in the subtle
nuances of preferential attention or lack of interest” (321). Thus a TRI or
CTRI can be ineffective, even harmful.
Consider,
for example, the meta-verbal qualities that would be required to make the
following interpretation benevolent: “I see you don’t care
about what I just said. You ignored it, which is kind of a devaluing thing to
do” (Carsky & Chardavoyne, 2017, 402). Which tone of voice? Which facial
expressions? Which accompanying gestures?
Using Transference and Countertransference Interpretations
Appropriate Versus Inappropriate Clients
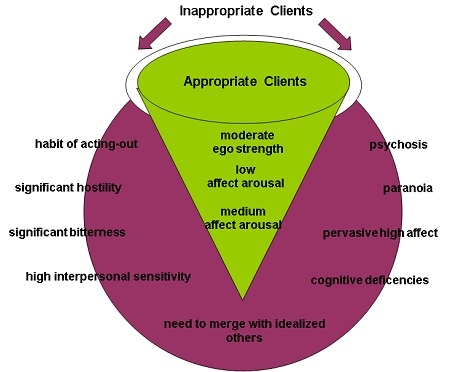
Therapists increase their chances of using
TRIs and CTRIs efficaciously when they keep in mind the characteristics of
their clients. Though recognizing those who can benefit from these
interpretations is far from easy, two fundamental principles are useful.
First, TRIs and CTRIs are appropriate only
“within the omnipotence of the patient, which has to be challenged sensitively
and very, very cautiously” (James, 1960, 289). TRIs and CTRIs are to be used
with clients who are open to them, ready for them, and able to benefit from
them (Steiner, 1993).
Second, TRIs and CTRIs are generally
appropriate with clients who have at least moderate ego-strength and
low-to-medium levels of affective arousal. Though they may be temporarily hurt
or angered by what they hear in an interpretation, they can use higher-level
defense mechanisms to alleviate their pain. They can avoid, in particular, the
use of the splitting defense that labels them as “all bad” and prevents them from
discriminating, relativizing, and accommodating to disturbing information.
Moreover, they can use their
reality-testing capacity to distinguish between what is intruding from the past
and what is being experienced in the present. They can counteract their
tendency to confuse facts with feelings. They can subject perception to
rational scrutiny. They may be temporarily impaired in interpersonal
functioning, but – given a little time to process their feelings and thoughts –
they can recover.
It is helpful in this regard to consider
personality traits as defined in the DSM-5-TR. A trait such as suspiciousness may
cause clients to have a difficult time at first when confronted with a TRI or
CTRI that brings to light their contribution to a therapeutic relationship
problem. But because their suspiciousness is neither persistent nor inflexible,
they can trust their therapist enough to give the interpretation due
consideration. Their functional impairment and subjective distress do not reach
the threshold of a personality disorder (APA, 2013, 648).
At the same time, personality disorders do
not categorically rule out the use of TRIs and CTRIs. For one thing, specific
personality traits and disorders of clients shape
transference-countertransference patterns in therapy (Blatt & Shahar,
2004). “Specific personality traits of [clients] are associated with different
countertransference reactions in therapists” (Hennissen et al., 2019). Personality
pathology in clients is related to qualitatively different countertransference
patterns in therapists (Colli et al., 2014). Furthermore, therapists should not
stop with diagnoses when considering interventions that are likely to be
efficacious. They must also consider a client’s ability to trust a therapist,
maintain a working alliance while exploring transference phenomena, and control
impulsivity (Colli et al., 2019).
To say this, however, is not to imply that
TRIs and CTRIs are appropriate in a given session. For
there will be times when highly aroused, suspicious clients, albeit those with
moderate ego-strength, simply need to be listened to and allowed to process
their strong feelings in their own defensive way. Even if that takes the entire
session, therapists should refrain from interpreting transference and
countertransference.
Specific highly charged emotions that
generally rule out TRIs and CTRIs include hostility, bitterness (Pick, 1997),
and paranoia accompanied by high levels of interpersonal sensitivity (Lasky,
1990). When clients are experiencing these powerful negative emotions or
attitudes, they are functioning in an
autistic, infantile-omnipotent manner. They have temporarily regressed to an
earlier developmental stage. They are too debilitated to tolerate participative
interventions such as TRIs and CTRIs. They will hear them as invasive, blunt,
and personal (Searles, 1975). At least for the time being, they must defend
their reputation for righteousness through denial, rationalization,
intellectualization, and other defense mechanisms.
In contrast, clients with at least
moderate ego-strength sometimes do not need an entire session to lower a
relatively high level of affective arousal and cognitive impairment. Because
they are not in the habit of relying solely on primitive defenses like
splitting or do so for only a short time, they routinely return to more
discriminating cognitive functions. They thereby process their negative affect
at least to the degree that their hostility is replaced by anger or irritation;
their bitterness, by disappointment; and their paranoia, by mild suspicion or
wariness. They do not have to cling to a reputation of being all good, for example,
and be angry about being thought less of. They can rationalize what they did,
admit the possibility of being somewhat in error, and be simply irritated both
with themselves and with those who have judged them.
On the other hand, clients with moderate
ego-strength and generally low levels of affective arousal who bring to therapy
embarrassing or highly sensitive issues may sometimes benefit from TRIs and
CTRIs. Through exploring not only how they feel and think when talking with
their therapist but also how their therapist feels and thinks, they can come to
see that others are not actually despising them or looking down upon them.
Rather, common humanity draws from others’ understanding and compassion. At the
same time, therapists are wise to take these clients’ repeated defensiveness,
noticeable opposition, or prolonged passivity as indications that they are not
ready for interpretations.
Similarly, when clients repeatedly or
strongly reject material, more often than not they are indicating that their heightened
arousal prevents them from thinking clearly. They do not have the capability to
manage their feelings. Especially if clients are highly internalizing and feeling
awkward, TRIs and CTRIs will intrude on their fragile mental capacities. They will
feel invasive.
For instance, clients who already feel
deeply rejected by a significant other can hear such a TRI as “You are refusing
to let me in on your pain” as simply critical of them. The interpretation can
indicate that they are being rejected because they are protecting themselves so
staunchly from their therapist’s efforts to help them. “I must be accepted for
doing so,” these clients will reason, “because I cannot risk intimacy. It
reminds me of the intimacy that I have lost. It can lead to more rejection.”
When this is the case, therapists must simply listen and reflect without
referring to transference or countertransference.
Even highly externalizing clients with
moderate ego-strength need help with symptom reduction and skill building
rather than with insight and relationship work when they are under great
stress. Though they are in the habit of sharing their emotional life, they are
feeling too vulnerable to do so at the time. Although they may benefit from a
carefully timed TRI or CTRI, they need externalizing interventions such as paraphrasing
and summarizing (Beutler, 2000).
Other clients generally unable to make
good use of TRIs and CTRIs are those who lack ego-strength or suffer other
serious deficiencies, such as pervasive, high levels of affective arousal. They
are emotionally unable to tolerate the honest feelings and thoughts of their
therapist; they are unable to process them. Especially if they were parented by
a mother who saw them as simply her narcissistic object or projection of her
own feelings, they see others as basically identical to themselves and, consequently,
cannot separate their own feelings from those of their therapist (Bach, 2019). TRIs
or CTRIs could even harm them.
Similarly, clients with a strong need to
merge with idealized others cannot usually tolerate working with limited,
vulnerable therapists, as is sometimes revealed in their CTRIs. Clients with
strong narcissistic tendencies, for example, need to bolster their sense of
self-worth by being worthy of only those therapists who are obviously capable.
For this reason, Kernberg (1975) warns against challenging an idealizing
transference, at least in the beginning phase of therapy. Instead, therapists
might simply ask for clarification.
Clients with dual diagnoses are also on
the list of those who do not ordinarily have sufficient ego functioning to work
with TRIs and CTRIs. They include those with long-term alcohol and drug
dependence, those who habitually act on their antisocial or suicidal impulses,
and those without the mental capacity to see connectedness (Crits-Christoph
& Barber, 1991; Pollack & Horner, 1985; Davanloo 1990).
Clients with a lower-level borderline
personality disorder present yet other problems. They have been found to
benefit from TRIs in particular (Kernberg, 1975; Levy & Scala, 2012). But because
they are habitually inclined to act out their feelings and impulses, they are
likely to perceive CTRIs as counter-assaults. They simply cannot appreciate
them “as therapeutically meaningful [statements] offered in good faith, because
such things are not expected from one’s most immediate enemy,” (Epstein, 1977,
461) albeit one’s most perfect friend minutes before – even if he or she is a
therapist.
Kernberg (1975) thinks that clients with a
lower-level borderline personality disorder do not do well with CTRIs because
they either distort them or simply cannot put them to use. Their core self is
composed of parts of others, adds Searles (1979), especially early in therapy.
More often than not, they experience a heightened affective arousal (Swift
& Wonderlich, 1990) that interferes with the cognitive work necessary for
processing interpretations.
Instead of using CTRIs with clients with a
lower-level borderline personality disorder, therapists are wise to simply
clarify the way these clients use splitting and other defenses and thereby
distort perceptions. Rather than focusing on their clients’ interpersonal
patterns, therapists are wise to slowly and indirectly resolve their resistance
to doing so (Spotnitz, 1976).
If, on occasion, therapists interpret
transference and countertransference to clients with a lower-level borderline
personality disorder, their TRIs and CTRIs should ordinarily refer not to
generic material (Volkan, 1995) but to the here-and-now. They might say, for
example, “It’s hard for you to share your bad experiences” rather than “It’s
always been hard for you to trust others enough to share your bad experiences.”
This focus will enable therapists to supply corrective data in concrete detail
as soon as they note their clients’ perceptual distortions. Alternately,
therapists might say, “I wonder what has prevented you from saying anything for
half an hour” and add, “Do I come across as criticizing you?”
At
times, however, even highly disordered persons can benefit from CTRIs. An
example would be the autistic child client that Franch (1996) describes as
unable to overcome two-dimensionality and relate to a world without meaning.
Because the autistic child can experience neither inside nor outside, Franch
approaches him exclusively from his countertransference. Using his own
feelings, sensations, fantasies, and associations to get information about the
client’s state of being, Franch assigns meaning to these data, communicates it
through CTRIs, and achieves a positive outcome. The child’s “frozen” internal
world gradually begins to “thaw,” and his transference arises in response to
his therapist’s countertransference.
Timing
After identifying clients who can benefit
from TRIs and CTRIs, therapists must still ask when and how often or with what
frequency they should use interpretations (Piper et al., 1993).
Joyce and others (1995) state that timing
depends on clients “inviting” their therapists to interpret. They “invite” when
they are ready. They can give up their defenses, focus inwardly, and find
personal significance in the interpretation. They can begin to process affect
connected with it.
Even so, it may be easier to identify
times when TRIs and CTRIs should not be used. One is when clients are
already dealing with significant past conflict. Ordinarily they should not
divert their attention to the therapist-client relationship if they are
exploring a destructive pattern outside the therapeutic setting (Pearson,
1995). On the other hand, therapists can be on the lookout for transference
data that persists after that work seems finished, for that unresolved
conflictual material would indicate a need for additional work.
Similarly, it would ordinarily be inappropriate to use TRIs and CTRIs when clients are already dealing with highly intrapsychic material, such as death, significant rejection, or humiliation, and are experiencing heightened raw emotion (Thornon, 2023). Simply listening respectfully and reflecting the client’s pain
would be better.
However, if the way the clients
choose to share their experiences causes problematic negative reactions in
therapists – reactions of which the clients are virtually unaware – therapists
might consider using TRIs and CTRIs. They might say, for example, “Your
shouting is scaring me into focusing on harm that might come to me instead of focusing
on your pain.”
Finally, therapists should be very careful
with using TRIs and CTRIs when clients are dealing with material too primitive
for language: when they cannot “give voice” to what they were experiencing. If
clients cannot give information, talk slow enough to be understood, or speak
coherently, TRIs and CTRIs exposing those phenomena might only deepen their frustration.
Rather, attentive silence or short affective responses that prepare clients to focus on transferential and countertransferential affect would be good choices. “Silence [in particular offers] clients a space for deeper awareness,” (Montgomery et al, 2023, 2). “It is a unique space for processing content related to transferences and countertransferences,” (2). It soothes and calms clients who can grasp only fragments of a painful experience. They would then be better able to share what is only partially known (Bollas, 1987). They would feel safe and secure enough in time to bring partial awareness to fuller consciousness, after which they might be able to explore their relationship with their therapist.
Frequency
A general, research-based rule is that
TRIs should be used infrequently rather than frequently (Piper et al., 1991;
Hoglend, 1993; Joyce & Piper, 1993) because other interventions are often
equally appropriate or more appropriate. The same rule is even more applicable
to CTRIs, which have an even greater potential than TRIs to divert attention
unnecessarily from clients’ presenting problems. TRIs and CTRIs should be interwoven
with active listening, explorations, clarifications, confrontations, and other
interventions (Bond et al., 1998; Bogwald et al., 1999; Grunebaum, 1986). Neither TRIs nor CTRIs should be used in place of supportive
interventions when they are needed.
The insight of Harry Stack Sullivan (1954)
is priceless. Because the supply of interpretations is greater than the demand,
the needs of clients must always take precedence over therapists’ desire for
insight and thus their use of an intervention they prefer.
Principles Underlying Guidelines for Using TRIs and CTRIs
Therapists will benefit from basing their
use of TRIs and CTRIs on the following therapeutic principles.
First, specific interventions depend on
the soundness of the therapeutic alliance. TRIs and CTRIs might lead to clients
using intellectualization and other defenses against resolving transference
conflicts if they are not comfortable in their relationship with their
therapist (Brenner, 1982).
In other words, TRIs and CTRIs should be
used after more supportive interventions (Gabbard et al., 1994). Clients
must feel accepted and valued in their therapy before they can examine how they
are contributing to interpersonal failures. CTRIs will be experienced as
premature if clients are suffering from intense guilt related to not fulfilling
their responsibilities. They will react with intensified guilt if therapists
intimate that they are not finding sessions helpful. They cannot accept
responsibility for their therapists’ mental states, even if they are occurring
in therapy (Searles, 1975).
Second, specific interventions should
deepen and maintain the therapeutic alliance. Thus TRIs and CTRIs can be used
if they will help clients discover that their unprocessed feelings toward their
therapist are creating an impasse in therapy. Used carefully, these
interpretations can facilitate clients’ trust and respectful acceptance of
their therapist. Thus they can mediate and moderate a solid, increasingly
meaningful therapeutic alliance.
Third, specific interventions should
repair a ruptured therapeutic alliance or a faltering working alliance. When
therapists have made a mistake and notice their clients’ corresponding
distress, they might need to use a CTRI such as, “You seem disappointed in me
because of my insensitive remark. Am I correct?”
Fourth, specific interventions should
address resistance to working on extra-therapeutic problems identified in
clients’ goals (Brenner, 1982). TRIs and CTRIs must not replace confrontation,
for example, when it is needed. They can be very useful, however, if what
clients are doing in therapy is precisely what they routinely do outside of it.
In sum, TRI’s and CTRI’s have been found to be clinical useful when therapists know how and when they should be used (Antichi and Giannini, 2022).
Final Thoughts
Admittedly, attempting to meet eleven
criteria for wording TRIs and CTRIs is a challenging undertaking. So is
deciding when, how often, and with which clients to use TRIs and CTRIs.
For
this reason, therapists are wise to remember that the more they use
TRIs and CTRIs without being harsh critics of themselves for making minor
errors in wording, timing, and frequency, the more adept they will become. Furthermore,
the more they simply observe and wonder about the tasks and functions they are
performing, the more relaxed they will become. They will thereby inspire their
clients to model themselves after them. Clients will realize that they, too,
can become accepting of themselves. They can be non-judgmental as they take personal
responsibility for their well-being. They can do work they have never done
before, work whereby they change themselves.
In other words, the goal of psychotherapy is
for clients to consciously play the roles that should have been played, but
were not, by others. For that is the only way they can resolve the conflicts they
have been unconsciously repeating or re-enacting. This implies, of course, that
therapists have the responsibility to create the conditions under which clients
can accomplish their goal, starting with dealing efficaciously with transference
and countertransference phenomena.
Finally, though some of the above
guidelines and principles might seem more precautionary than not, they are not
intended to diminish the potential of TRIs and CTRIs to contribute to
a successful outcome. The therapeutic and working alliances in particular benefit
significantly from the candor, immediacy, and honesty of these interventions. When
used sensitively and prudently, TRIs and CTRIs serve as powerful mediators and
moderators of positive therapeutic outcome (Andersen & Przybylinski, 2012; Antichi & Giannini, 2022).
Footnotes
(Note: To return to the course after having clicked a footnote, click the Back button in your browser.)
Note 1. Clients
somehow know when their therapists are open to connotation-carrying displaced
material. They sense that it is safe to put into words what they suspect is
furthering or hindering their well-being. When therapists are not open to the
possibility of countertransferential communication, by contrast, clients do not
feel safe enough to do so (Kantrowitz, 1997).
Note 2. It can be argued that when clients bring in extra-therapeutic material for the sake of dealing with out-of-session problems, it is more appropriate for therapists to accept it at face value and teach clients skill building. With this approach, however, the question remains as to whether those skills are actually used outside of therapy. Clients describing their behavior may be merely relating how they hoped they acted. On the other hand, when therapists admit the possibility of the transferential meaning of extra-therapeutic material, they pave the way for making the therapeutic setting itself a venue for interpersonal skill building. As they get first-hand experience of clients’ transferential behavior, therapists can all but guarantee skill acquisition.
Note 3. By
comparison, when clients treat their therapists as if they were third parties,
they may be displacing away from their therapists. They may be
expressing their feelings, attitudes, and impulses toward third parties. It is
likely that they are doing so because they have recognized themselves behind or
in these extra-therapeutic persons and wish to reveal who they are by referring
to the third parties (Giovaccini, 1967). When this is the case, if therapists
are to discover the interpersonal styles of their clients, they must also
decode this non-transferential material.
Note 4. The
concept of transferential feelings implies that the experience of
similarity initiates the affect rather than the affect initiating the
experience of similarity. However, it is more likely that either both are
initially operative or the distinction is artificial. The feeling imbues the
experience just as the experience imbues the feeling.
Note 5. Of the
feelings striving for expression, fear appears to be the most pervasive.
Consequently, it is the most common transference affect. At times, clients
transfer to their therapist hostile behaviors and qualities that inspire fear.
At other times, they let basic fear create the appearance of threatening
behaviors and qualities in the therapist, for while early
parental figures were nurturing and life-sustaining, they were also capable of
withdrawing that care and sustenance at any time. Indeed, they held what felt
like absolute authority and appeared to require clients to please them to win their love. If parents were displeased, their negative attention could
inspire only fear. Thus clients knew no middle ground, softened emotions, or
counteractive forces. All was primitive: all-good or all-bad.
Note 6. Depression
is regarded as a major form of acting-in because the anger and anxiety at its
core are being turned inward and directed toward the self. Because these two
emotions are less responsive to inhibitory efforts that reduce the likelihood
of acting-out, therapists unconsciously conceal them in depression.
Note 7. Therapists
are wise to decode their feelings of being punished to uncover their
possible anger-base even though they can explain neither the exact nature of
the punishment nor the reason for it. It may be that in punishing their
therapists, clients are asking them to respond positively to a negative
experience. They are hoping to revise their beliefs about themselves and their
interpersonal worlds through witnessing their therapists return good for evil.
On the other hand, therapists’ feelings of being punished may stem from their being taken for granted, used, or abused. They may resent having to give precious time to clients whose issues seem mundane in comparison with the horrific issues of other clients. After therapists have worked with sexual abuse victims or have been victimized themselves, for example, they may find it difficult to appreciate clients’ distress resultant from a minor setback.
Note 8. To a
certain extent, of course, anxiety is characteristic of all
countertransferential reactions, for in the process of being impacted by
clients’ transference, therapists lose cognitive control (Kantrowitz, 1997).
Rarely, however, are they conscious of losing it.
Note 9. Therapists
may rationalize their tendencies by saying that their clients need their
insight. But more likely than not, therapists are discounting their clients’
insight more than adding to it (West & Schain-West, 1997).
Note 10. Because
clients often conceal their fantasies and daydreams, methods like Eye Movement
Desensitization and Reprocessing (EMDR) (Shapiro, 1995) are invaluable
interventions. When bilateral movement sets stop and clients are asked “What is there now?”, therapists often become privy to transferential fantasies that clients would not otherwise share.
Note 11. Space and time do not permit a full exploration of why the body reveals transferential truth, indeed why it cannot lie. But research suggests that memory is spread throughout the body in wavelike frequency patterns along a network of fibers on all nerve cells rather than stored in specific cells or cellular tissues. Memory capacities, therefore, exist not just in cerebral neurons but in all parts of the body’s nervous system, and not just in the nervous system but in all cellular tissues of the body (Oschman & Oschman, 1995b). Furthermore, because the body is a continuous, unbroken fabric and a living matrix, throughout its entire system it retains a “record or memory of the influences that have been exerted upon it, both as an individual and as a member of the [human] race” (Oschmann & Oschmann, 1995a, 65). The body remembers both ancestral information through genetic transmission and personally experienced events (Schacter, 1996). Because of this highly developed capacity, the body is constantly responding to present stimuli against a background of past experiences. Cells are being reminded of previous similar experiences, from simple sensations to highly structured cognitions that give events meaning.
Note 12. Some theorists assert that all therapeutic behavior, including verbal behavior, is motivated by and reflective of transference and countertransference (McLaughlin, 1990). Most, however, find that only some therapeutic behavior is rightfully connected to transference and countertransference. Clients may come late, for example, not because of early familial patterns but because of resistance to being in therapy in the first place, no matter how little their therapist reminds them of a parent. Thus therapists must at times discontinue decoding or choose not to begin engaging in it.
Note 13. Research reveals that body language or simple movement may prove beneficial to clients and contribute to positive outcome if it is truly a response to clients’ attachment affect, namely sadness, fear, and anger (Dreher et al., 2001). On the other hand, simple movement may be harmful to clients and contribute to negative outcome if therapists simply match the behavior of their clients. Therapists’ smiling back, for instance, appears to be especially harmful when clients are feeling shame in addition to anger. Therapists may consciously intend to strengthen the therapeutic alliance by smiling even while feeling angered by what they hear from clients. Unconsciously, however, therapists may be denying the degree of their anger. In addition, their smiling may be countertransferential in that therapists have themselves learned to smile when anxious about expressing their anger. Hence, therapists’ responsibility to decode such a phenomenon as their urge to smile.
Note 14. Clients who lean forward may be indicating that they have come to trust their therapist enough to share intimate information. In contrast, clients who remain chair-bound may be “saying” that they are uncomfortable with revealing what is humiliating.
Note 15. Although
it is appropriate on select occasions to show feelings in action, if doing so
is the only method in clients’ repertoire, they may need to discover that
acting-out usually creates a minefield of negative interpersonal relationships.
Note 16. Transference
enactments fall into two categories depending on how therapists respond to the
roles they are assigned (Levin, 1997). In the first and more common category,
therapists actually assume the role they are being assigned and thus fulfill
their client’s transference expectations. In the second, therapists refuse that
role and thus fail to meet their clients’ expectations. In fact, to
help their clients realize that they are living not in the past but in the
present, where they must assume responsibility for their own self-care,
therapists may have no other choice but to decline their role assignment.
Note 17. Factors
increasing the likelihood of countertransferential enactments originating in
therapists are permeable boundaries, poor impulse control, inadequate
education, excessive therapeutic zeal (Searles, 1979), and blind spots (Plakun,
1998).
Note 18. Factors increasing the likelihood of countertransference enactments triggered by clients are certain personality disorders and the use of primitive defense mechanisms. For example, clients may replay the trauma that they are suffering outside of therapy by assigning roles of victims to themselves and abusers to their therapists. Or they may become abusers themselves and make their therapists victims.
Note 19. Whatever
their specific form or immediate cause, countertransferential enactments must
be decoded lest they cause the therapeutic focus to shift unnecessarily from
what clients need to achieve to how they are relating to their therapists. If
clients’ conflicts with their therapists closely resemble those with
non-therapists, all is well. If not, however, clients must use precious time
and energy dealing with the disconnectedness that has ruptured their
relationship with their therapist instead of exploring their own issues.
Therapists who are overly sensitive to slights, for instance, can revert to
defending their treatment-related actions and blaming clients for not
cooperating with them when clients complain that therapy is not benefiting
them. Having to focus on their therapists’ powerful defensive feelings, clients
are not able to explore the negative feelings that explain why treatment is not
working.
Note 20. The same
kind of failure can result from therapists’ insistence that clients are not and
never were responsible for such a thing as participation in sexual abuse as
children. Therapists may do so in the name of reality testing, Plakun (1998)
explains, but they thereby prevent clients from processing the painful feelings
of guilt that some sexual victims carry.
Note 21. This
response contrasts with silence that is appropriate when content loses its
importance or when interpreting strikes clients as nagging or doing something
they could do themselves (Bird, 1922).
Note 22. It also
appears as if the human brain can exploit what are called holographic
principles. Each part of the brain can contain both a fragment of a memory and
the entire memory in miniature. Consequently, association upon association is
possible, with every cellular tissue capable of “revealing” the truth the whole
person “knows” (Pribram, 1971). Thus somatic memory may indeed hold the “truth”
about what clients have displaced from significant, pre-therapy and
extra-therapy persons to their therapists.
Note
23. The clinician’s primary function is as an affect regulator for the client’s
primitive, traumatic states, including those that are walled off by
dissociation. (Schore, 2003a, 246). Dissociation, the blocking of the path
between the limbic system and the cortex, is an early-appearing, very primitive
defense against traumatic affects that are stored subcortically in the right
hemisphere.
Note
24. Bion (1967) suggests that containing is required because the clients’
mothers’ capacity to contain the clients’ distressing emotions was
insufficient. They were therefore returned to the clients little changed and
difficult to integrate. The mothers were unable or unwilling to provide a model
for the clients’ containment of their own feelings; this the therapist must do.
Note 25. As Gilboa
and Revelle (1994) explain, “The longer the period during which a person is
influenced by physiological and cognitive processes activated by emotion, the
higher the probability that this experience will be subjectively perceived as
important and meaningful”(135).
Note 26. Because
early relational trauma is stored in the right hemisphere, therapists choose to
engage in right brain-to-right brain emotional communication. They refrain from
using their left brain to put their experience into words. Instead, they tolerate
uncertainty, for it is fundamental to a healthy growth process. Even though it
is anxiety-producing, it is an opportunity for change (Schore, 2003a). It is an
opportunity for clients to create something out of themselves (Balint, 1968).
By contrast, if therapists block their own negative somatic markers by shifting
out of their right brain into their left brain, they cut off their empathic
connection to their own pain and therefore to their clients’ pain. If
therapists speak quickly, their clients are likely to perceive them as critical
(Ryle, 1994).
Note 27. These are false assumptions because only by holding clients’
transference can therapists facilitate an expansion of clients’ narrow personal
psychological space and collaborate with them to fashion what is real, in
contrast to what they want to be real (Slochower, 1999).
Note 28. By
containing and eventually processing transference, however, therapists
facilitate a detoxification process whereby clients’ unwanted transference
projections lose their potency. By the course of holding transference,
therapists really know their clients well enough to help them make transference
a resource under the control of their reality-testing ego. By holding
transference, therapists and clients together strip displaced material of its
dangerous, uncontrollable pathogenic elements and make it simply a memory
residing in the unconscious mind (Grinberg, 1997).
Note 29. This is
very difficult for therapists because of a delay between clients’ projection of
unwanted traits and therapists’ becoming conscious of what has happened. In the
interval, therapists can easily act in accordance with the traits or at least
be disturbed by the feelings they stimulate. They find it hard to hold or
contain their clients’ painful feelings and allow their clients’ experience to
fully impact them (Roth, 2001). They desire to defend against an awareness of
the projection and its painful feeling. They act them out to get
rid of them.
Note 30. If feelings of success during a session are
due primarily to clients’ transference, the therapist’s work might entail
helping them realize that their wanting to sustain a positive therapeutic
relationship is making them reluctant to reveal facets of their lives likely to
inspire disgust or dislike in their therapist. This, in turn, might result in
wasted therapeutic effort. On the other hand, if feelings of success during a
session are due primarily to therapists’ displaced attitude, they may need to
manage their feelings carefully in order to stay attuned to the feelings of
their clients, which are often those of failure. Should therapists allow their
good fortune to become more important to them than their clients’ feelings of
deprivation or misfortune, clients may have yet another poignant experience of
being compared to others and found wanting.
Note
31. Self-monitoring adds conscious processing of countertransference to
intuition and other unconscious mental operations (Arlow, 1985).
Note 32. Neither
may therapists end the session early simply because feelings of hatred have
become too strong for comfort, for while this solution might be helpful in the
short run, it is harmful in the long run in that it implies that hatred is too
unmanageable to be contained in the therapeutic environment. If hatred cannot
be contained in the therapeutic environment, by inference it cannot be
contained anywhere. It must be staunchly repressed, which only increases its
power.
Note 33. In terms of the right brain,
therapists shift up and down between its higher and lower levels: those
connected to cognition and those connected to emotion (Schore, 2003b).
Note 34. However central clients are to the therapy “product,”
therapists must remain the heart of the therapy “process.”
Note 35. Readers
will note that TRIs and CTRIs are being defined in accordance with the operational
definitions of transference and countertransference. It is especially important
to note that TRIs and CTRIs need not refer directly to the unresolved
conflictual relationships being transferred to the therapy relationship.
Rather, they can simply identify a therapist-client conflict that is available
for immediate and concrete examination. Later, if it is in the interest of the
client, the therapist and client can explore the original experiences that lay
the groundwork for the therapist-client conflict.
Note 36. This is extremely
challenging, of course, for when therapists unconsciously assume the roles that
their clients have transferred, they experience in themselves strong, even
intense, countertransference attitudes and feelings (Diamond, 1989). Therapists
fear clients’ anger. They are disturbed by clients’ erotic, dependent, or
sadistic feelings and frightened by clients’ desires to merge with them or to
humiliate them. They are anxious about clients who have become victims of abuse
and worried about how much their clients can take (Pick, 1997; Wallerstein,
1990). At times, therapists even worry about how much they themselves can take:
how many times they can be asked to take with impunity roles of harsh authority
figures, of victimizing sibling figures, and on and on. Concurrently, they
wonder how many times they can unconsciously dredge up their own memories of
painful interpersonal relationships brought to mind by their clients’
self-revelations.
Note 37. One might
argue that if clients are not calm, TRIs should be reflective of that state. If
therapists attempt to calm disturbed clients immediately, they give them the
message that their disturbing feelings are not acceptable. While this point is
well taken, responding to heightened, unprocessed emotional disturbance in kind
is not as therapeutic as those who are disturbed would like to believe. It is
not the harboring of disturbance that is healing but the recognition,
containment, and interpretation of it. It is new and different thinking that
both serves as a basis for remedial action and leads to an emotion’s demise.
Note 38.
Especially in the realm of sexual abuse, therapists must make TRIs emotionally
immediate. If they wait too long to interpret material, clients can experience
therapists as being afraid to face facts. Therapists can appear to be
re-enacting like someone who turned a blind eye to what was happening
(Casement, 1991). The timing of TRIs is crucial, however, because immediacy must be
tempered by emotional readiness on the part of both clients and therapists.
TRIs referring to sexual abuse, in particular, must not be spoken too soon,
lest clients experience therapists as either voyeuristic or uneasy with the
material.
Note 39. When clients use strong terms or
exaggeration to describe others, they make therapists wonder if their clients
are also referring to them, which makes it more difficult for therapists to
remain ego-based and neutral. “My mother is a witch!” an adolescent might cry
soon after a therapist sets limits on the client’s behavior. To maintain
neutrality and calm and yet keep the TRI emotionally immediate, the therapist
might reply, “You put great emphasis on how your mother seems to you to be a
witch. Are you experiencing someone – maybe me – as being mean to you?” In
using phases like these, therapists play back clients’ descriptions as clearly their perception, rather than both theirs and their therapists.’ Thus therapists
keep a balance between respecting clients’ points of view as subjectively valid
and questioning their objective validity, their being defenses against reality
rather than facts. Therapists remain neutral at the same time that they note
the forcefulness and immediacy of clients’ feelings.
By contrast, if clients talk about their
“shitty feelings” and therapists also refer to their “shitty feelings,” clients
might be relieved to hear their therapists accept their viewpoint. But they
might also hear in the interpretation, “Your feelings really are shitty” and
consequently not examine feelings that they themselves may question.
Indeed, further questioning seems unnecessary if clients’ descriptions and
perceptions have been accepted as accurate by their therapists. By contrast,
“You have come to regard your feelings as shitty. How did this come about?”
gives clients the psychological space within which to examine their feelings.
Similarly, a TRI that invites further examination, such as “I think you expect
me also to see your feelings as shitty,” permits clients to hear a helpful
reflection (Casement, 1991).
Note 40. Neutrality is
especially important when clients give their therapist negative feedback about
a TRI, such as their feeling criticized because of it. “It is harmful … when
[therapists] appear to ignore clients’ accurate perception or interpret
defensively in the face of it” (Casement, 1991, 131). Focusing first and only
on the transference could strike clients not only as therapists’ being
defensive but also as their denying the elements of objective reality in their
relationship. It could be detrimental to the working alliance to say to a
client something like “I wonder if you see me as critical because I resemble
your critical father” (Casement, 1991).
Instead, therapists might simply
acknowledge the reality, saying, for example, “I can see how you could have
heard what I said as critical.” In some cases, therapists might also add, “I
must have sounded critical.” They would thereby be acknowledging the client’s
feelings but not admitting doing something that justifies those feelings.
Note
41. In some instances, if a positive therapeutic outcome is to be achieved, TRIs
must focus not just on defenses or resistance. Therapists must also refer to
clients’ wishes and fears (Winston et al., 1993). For example, if a client were
speaking of a third party as especially supportive, the transferential message
to the therapist could simply be a wish that the therapist was similar. The
client could simply be signaling that there is a conflict between what is being
experienced and what is hoped for and that this conflict needs attention
(Casement, 1991). In such a case, the therapist should simply say, “Do you wish
that I would be more supportive of you also?”
At times, therapists should also refer to
the fear or anxiety which causes the defense or resistance. They might say, “It
seems as if you are extremely anxious about sharing about your past.
Could we look at what that anxiety is all about?” rather than “What is so hard
to share?” or “You seem so unwilling to share.” It is safe to focus on the
anxiety before the content accounting for the resistance, Klein (1952) assures
therapists who do not want to lose important content. The content associated
with the anxiety will not recede permanently; it will return.
However, there are times when clients must
be helped to cope with old, dangerous situations before they can even admit
their fears (Greenson & Wexler, 1969). Thus, a TRI such as, “You seem unable
or unwilling to share with me today. I wonder what might be going on,” would be
more effective than, “Could it be that you fear me today, that you see me as
your abusive mother?”
Note 42. Erotic transference, is often indicative of behavior that has become habitual and
pervasive. Thus a tentatively worded CTRI like the following may be especially
beneficial. “I could be wrong, but your flirting with me might be something you
do outside of therapy. Could we explore my suspicion?”
Note 43. It is also especially important
for therapists to use tentative CTRIs when they attempt to share an instinct,
Viederman (1974) explains, because it is an experience on the boundary between
the somatic and the psychic. And because an instinct is vague, obscure,
nameless, and barely outlined, a CTRI referring to it will be more effective if
worded tentatively.
Note 44. To be appropriately
inclusive, a therapist might say, “I wonder if you resent my not being pleased
with your progress. You would like me to say you have done enough to acquire a
new habit even though you really haven’t been consistent.” Or a therapist might
reflect, “Could it be that you fear my judgment so much that you exaggerate
your progress? Do you see me as a more important judge of your conduct than you
are?”
Note 45. The
following inclusive CTRI serves as an additional example of movement from
here-and-now to there-and-now. “My anger toward you may be similar to your
wife’s anger toward you, the anger you said you simply couldn’t understand.” So
does, “Could it be that my getting distracted when you talk too long is
reflective of what your wife does?”
Note 46. Time and space do not allow for a
fuller explanation of Ecker and his colleagues’ approach to resolving
intrapsychic conflict, but two of their books are listed in the reference
section.
Note 47. Therapists should also be wary of
their own tendency to see evidence of what they are expecting to find, for it
is human to relate to something familiar as if it were universal and
ubiquitous. “We do not have to be so quick to use old insights when we can
learn to tolerate longer exposure to what we do not yet understand. And, when
we do think we recognize something familiar from a [client], we need still to
be receptive to that which is different and new” (Casement, 1991, 29).
References
Aguayo, J. & Lundgren, J. (2018). I’m still alive. British Journal of Psychotherapy, 34, 194-198.
Andersen, S., & Przybylinski, E.
(2012). Experiments on transference in interpersonal relations: Implications
for treatment. Psychotherapy, 49, 370-383.
Antichi, L, & Giannini, Y. (2022). Interpretation in psychodynamic psychotherapy: A systematic review. Psychodynamic Practice, 28, 12-25.
Arlow, J. (1985). Some technical problems
of countertransference. Psychoanalytic Quarterly, 54, 164-174.
Bacal, H. A. (1990) Optimal responsiveness
and the specificity of self object experience. In H.A. Bacal (Ed.), Optimal
responsiveness: How therapists heal their patients (141-170).
Northvale, NJ: Jason Aronson.
Bach, S. (2019). The inner world, the gut,
and the sense of reality. Psychoanalytic Psychology. Advance online
publication. http://dx,doi.org/10.1037/pap0000256.
Bachant, J., & Adler, D. (1997).
Transference: Co-constructed or brought to the interaction? Journal of the
American Psychoanalytic Association, 45, 1097-1120.
Badcock, C. (2009). The imprinted brain:
How genes set the balance of the mind between autism and psychosis. Philadelphia,
PA: Jessica Kinsley Publishers.
Baker, R. (1993). The patient’s discovery
of the psychoanalyst as a new object. International Journal of
Psycho-Analysis, 74, 1223-1233.
Balamuth, R. (1998). Remembering the body:
A psychoanalytic study of presence and absence of the lived body. In L. Aron
& F.S. Anderson (Eds.), Relational perspectives on the body (263-286). Hillsdale, NJ: The Analytic Press, Inc.
Balint, M. (1968). The basic fault:
Therapeutic aspects of regression. London: Tavistock Pub.
Bauer, B. P., & Mills, J.A. (1989).
Use of transference in the here and now. : Patient and therapist resistance. Psychotherapy,
26, 112-119.
Becker, E. (1973). The denial of death. NY: The Free Press.
Bennett., K., & Clark, E. (2021). Crossing guardians: Signaling and safety in queer and trans therapist/patient dyads. Psychoanalytic Psychology, 37, 216-222.
Betan, E., Heim, A., Zittel-Conklin, C.,
& Westen, D. (2005). Countertransference phenomena and personality
pathology in clinical practice: An empirical investigation. The American
Journal of Psychiatry, 162, 890-898.
Beutler, L. E. (2001I). David and Goliath:
When empirical and clinical standards of practice meet. American
Psychologist, 55, 997-1007.
Bion, W. R. (1961). Experiences in
groups. London: Tavistock.
Bion, W. R. (1967). Notes on memory and
desires. Psychoanalytic Forum, 2, 272-273 and 279-280.
Bird, B. (1992). Notes on transference: Universal
phenomenon and the hardest part of analysis. Journal of the American
Psychoanalytic Association, 20, 267-301.
Blatt, S., & Shahar, G. (2004).
Psychoanalysis – With whom, for what, and how? Comparisons with psychotherapy. Journal
of the American Psychoanalytic Association, 52, 393-447.
Blum, H. P. (1986a). Countertransference
and the theory of technique: Discussion. Journal of the American
Psychoanalytic Association, 34, 309-328.
Blum, H. P. (1986b) Countertransference
and technique. Discussion. Journal of the American Psychoanalytic
Association, 34, 329.
Bogwald. K., Hoglend, P., & Sorbye, O.
(1999). Measurement of transference interpretations. Journal of
Psychotherapy Practice and Research, 8, 264-273.
Bollas, C. (1983). Expressive use of the
countertransference. Contemporary Psychoanalysis, 19, 1-34.
Bollas, C. (19887). The shadow of the
object: Psychoanalysis of the unthought known. London: Free Association
Books.
Bond, M., Banon, E., & Greneier, M.
(1998). Differential effect of interventions on the therapeutic alliance with
patients with personality disorders. Journal of Psychotherapy Practice and
Research, 7, 301-318.
Bonnet, G. (1991). Le transfert dans la
clinique psychanalytique. Paris: Presses University France.
Bostanov, V., & Kotchoubey, B. (2004).
Recognition of affective prosody: Continuous wavelet of event-related brain
potentials to emotional exclamations. Psychophysiology, 41, 259-268.
Boyer, L. B. (1997). The verbal squiggle
game in treating the seriously disturbed patient. In V.D. Volken and S. Akhtar
(Eds.), The seed of madness (155-176). Madison, CN: International
Universities Press.
Bradley, R., Heim, A., & Westen, D.
(2005). Transference patterns in the psychotherapy of personality disorders:
Empirical investigation. The British Journal of Psychiatry, 186, 342-349.
Brenner, C. (1982). The mind in
conflict. New York: International University Press.
Brodbeck, H. (1995). The psychoanalyst as
participant and observer in the psychoanalytic process: Some thoughts on
countertransference from a constructionist perspective. Psychoanalysis and
Contemporary Thought, 18, 531-558.
Bromberg, P. M. (1991). On knowing one’s
patient inside out: The aesthetics of unconscious communion. Psychoanalytic
Dialogues, 5, 55-71.
Brownstein, C. (2007). Kleinian theory. London, U.K.: Whurr Publishers.
Carsky, M., & Chardavoyne, J. (2017).
Transference focused psychotherapy and the language of action. Psychoanalytic
Psychology, 34, 397-403.
Casement, P. (1991). Learning from the
patient. New York: The Guilford Press.
Chammas, D. (2023). Different than me. Journal of Pain and Symptom Management, 00, 1-2.
Chasseguet-Smirgel, J. (1984). Creativity
and perversion. London: Free Association Books.
Chused, J. (1992). The patient’s
perception of the analyst: The hidden transference. Psycho-analytic
Quarterly, 61, 161-184.
Cohen, M. B. (1952). Countertransference
and anxiety. Psychiatry, 15, 231-243.
Colli, A., Gagliardini, G.,
Degl’Innocenti, B., Monti, M., & Foresti, G. (2019). What psychoanalysts do
in their everyday clinical practice: Empirically derived prototypes of the
psychoanalytic process. Psychoanalytic Psychology. http://.doi.org/10.1037/pap0000231
Colli, A., Tanzilli, Al, Dimaggio, G.,
& Lingiardi, V. (2012). Patient personality and therapist response: An
empirical investigation. The American Journal of Psychiatry, 171, 102-108.
Cooper, A. M. (1987). Changes in
psychoanalytical ideas: Transference interpretation. Journal of the American
Psychoanalytical Association, 35, 77-98.
Cooper, S. (1993). Interpretive
fallibility and the psychoanalytic dialogue. Journal of the American
Psychoanalytic Association, 41, 95-123.
Cowen, A., Elfenbein, H., Laukka, P.,
& Keltner, D. (2019). Mapping 24 emotions conveyed by brief human
vocalization. American Psychologist, 74, 698-712.
Cowen, A., & Keltner, D. (2020). What the face displays: Mapping 28 emotions conveyed by naturalistic expression. American Psychologist, 75, 349-364.
Crits-Christoph, P., & Barber, J. P.
(Eds.). (1991). Handbook of short-term dynamic psychotherapy. New York:
Basic Books.
Crowley, R. M. (1988). Human reactions of
analysts to patients. In B. Wolstein (Ed.), Essential papers on
countertransference (84-90). New York: New York University Press.
Damasio, A. R. (1994). Descartes’
error. New York: Putnam.
Davanloo, H. (1990). Unlocking the
unconscious. Chichester, England: Wiley.
DeLaCour, E. P. (1985). Aspects of
transference interpretation. Smith College Studies in Social Work, 56,
1-14.
Deutsch, H. (1926). Occult processes
during psychoanalysis. In G. Devereux (Ed.), Psychoanalysis and the occult (133-146). New York: International Universities Press.
Diamond, M. J. (1989). Stagnation, chaos,
and severe character neuroses. Psychoanalytic Psychology, 6, 455-473.
Dosamantes, I. (1992). The intersubjective
relationship between therapist and patient: A key to understanding denied and
denigrated aspects of the patient’s self. The Arts & Psychotherapy, 19, 359-365.
Dreher, M., Mengele, U., Rainer, K., &
Kammerer, A. (2001). Affective indicators of the psychotherapeutic process: An
empirical case study. Psychotherapy Research 11, 99-117.
Ducharme, E. Best practices in working with complex trauma and dissociative identity disorder. Practice Innovations, 2, 150-161.
Ecker, B., & Hulley, L. (1996). Brief-oriented
depth therapy. San Francisco, CA: Jossey-Bass.
Ecker, B., Ticic, R., & Hulley, L.
(2012). Unlocking the emotional brain. New York, NY: Routledge.
Epstein, L. (1977). The therapeutic
function of hate in the countertransference. Contemporary Psychoanalysis, 13,
442-461.
Evans, M. (2022). ’If only I were a boy…’: Psychotherapeutic explorations of transgender in children and adolescents. British Journal of Psychotherapy, 00, 1-17.
Fast, I. (1992). Developments in gender
identity: Gender differentiation in girls. International Journal of
Psycho-Analysis, 60, 443-453.
Ferder, F. (2010). Enter the story:
Biblical metaphors for our lives. NY: Orbis Books.
Ferenczi, S. (1909). Sex in
psychoanalysis. New York: Basic Books.
Field, N. (1989). Listening with the body:
An exploration in the countertransference. British Journal of Psychotherapy,
5, 512-522.
Finell, J.S. (1986). The merits and
problems with the concept of projective identification. Psychoanalytic
Review, 73B, 103-120.
Franch, N. (1996). Transference and
countertransference in the analysis of a child with autistic nuclei. International
Journal of Psycho-Analysis, 77, 773-786.
Freud, S. (1905). Fragment of an analysis
of a case of hysteria. Standard Edition, 7: 1-122. London: Hogarth
Press.
Freud, S. (1926). Inhibitions, symptoms,
and anxiety. In J. Strachey (Ed. & Trans.), Standard Edition, 20: 87-151. London: Hogarth Press.
Furlong, A. (2022). Establishing and maintaining a therapeutic frame. The Scandinavian Psychoanalytic Review, 3, 17-22.
Gabbard, G. O. (1994). Sexual excitement
and countertransference love in the analyst. Journal of the American
Psychoanalytic Association, 42, 1083-1106.
Gazzillo F., Curtis, J., Bush, M., &
Dazzi, N. (2019. Patients’ unconscious testing activity in psychotherapy: A
theoretical and empirical overview. Psychoanalytic Psychology, 36, 173-183.
Gelso, J., & Bhatia, A. (2012).
Crossing theoretical lines: The role and effect of transference in nonanalytic
psychotherapies. Psychotherapy, 49, 384-390.
Gelso, C. J., & Hayes, J. A. (1998). The
psychotherapy relationship. New York: John Wiley & Sons, Inc.
Gelso, C., & Hayes, J. (2007). Countertransference
and the therapist’s inner experience. Perils and possibilities. Mahwah, NJ:
Erlbaum.
Gene-Cos, N., Fisher, J., Ogden, &
Cantrel, A. (2016). Sensorimotor Psychotherapy Group Therapy in the Treatment
of Complex PTSD. Annals of Psychiatry and Mental Health, 4, 1080-1092.
Gilboa, E., & Revelle, W. (1994).
Personality and the structure of affective responses. In S. H. M. Van Goozen,
N. E. Van de Poll, & J.A. Sergeant (Eds.), Emotions: Essays on emotion Theory (135-159). Hillsdale, NJ: Erlbaum.
Gill, M. M. (1982). Analysis of
transference (Vol.1). New York: International Universities Press.
Giovacchini, P. L. (1960). On scientific
creativity. Journal of the American Psychoanalytic Association, 8, 407-426.
Giovacchini, P. L. (1967). Frustration and
externalization. Psychoanalytic Quarterly, 36, 571-583.
Gomberoff, M., Noemi, C., & De
Gomberoff, L. (1990). The autistic object: its relationship with narcissism in
the transference and countertransference of neurotic and borderline patients. International
Journal of Psycho-Analysis, 71, 249-259.
Gorkin, M. (1996). Countertransference in
cross-cultural psychotherapy. In R. Perez-Foster, M. Moskowitz, & R.A.
Javier (Eds.), Reaching across boundaries of culture and class: Widening the
scope of psychotherapy (159-176). Northvale, NJ: Jason Aronson.
Gorney, J. W. (1978). The negative
therapeutic reaction. Contemporary Psychoanalysis, 15, 288-337.
Greenson, R. R., & Wexler, M. (1969).
The nontransference relationship in the psychoanalytic situation. International
Journal of Psycho-Analysis, 50, 27-38.
Grinberg, L. 1997. Is the transference
fear by the psychoanalyst? International Journal Psycho-Analysis, 78, 1-14.
Grunebaum, H. (1986). Harmful
psychotherapy experience. American Journal of Psychotherapy, 40,
165-176.
Hafiz (Shams-ud-din Muhammad: 1320-1389
CE). (2011). “Haphazard brilliant thoughts.” In D. Ladinsky (Trans.), A year
with Hafiz: Daily contemplations, (p. 233). NY: Penguin Books.
Handley, N. (1995). The concept of
transference: A critique. British Journal of Psychotherapy, 12, 49-59.
Heath, S. (1991). Dealing with the
therapist’s vulnerability to depression. Northvale, NJ: Jason Aronson.
Hedges, L. (2007). The organizing
transference and psychotic signifiers. Psychologist-Psychoanalyst, Fall, 21-25.
Hennissen, V., Meganck, R., Van
Nieuwenhove, K., Norman, U., Loeys, T., & Desmet, M. (2019). Therapists’
responses toward dependent (anaclitic) and self-critical (introjective)
depressed outpatients: A multilevel approach. Psychotherapy, 52, 1-12.
Hinshelwood, R. (1999).
Countertransference. International Journal of Psycho-Analysis, 80, 797-818.
Herron, W. G., & Rouslin, S. (1982). Issues
in psychotherapy. Washington, DC: Orgin.
Hinshelwood, R. (1999).
Countertransference. International Journal of Psycho-Analysis, 80, 797-818.
Hoglend, P., & Hagtvet, K. (2019).
Change mechanisms in psychotherapy: Both improved insight and improved
affective awareness are necessary. Journal of Consulting and Clinical
Psychology. http://dx.doi.org/10.1037/ccp0000381.
Hubble, J. (1999). Novel drugs for
Parkinson’s disease. The Medical Clinics of North America, 83, 525-536.
Isakower, O. (1963). Minutes of the New
York psychoanalytic institute faculty meeting, October 14 (unpublished).
Jacobson, J. G. (1993). Developmental
observation, multiple models of the mind, and the therapeutic relationship in
psychoanalysis. Psychoanalytic Quarterly, 62, 523-552.
James, M. (1960). Premature ego
development: Some observations on disturbances in the first three months of
life.” International Journal of Psycho-Analysis, 41, 288-94.
Joyce, A., & Piper, W. (1993). The
immediate impact of transference interpretation in short-term individual
psychotherapy. American Journal of Psychotherapy, 47, 508-526.
Joyce, A., Duncan, S., & Piper, W.
(1995). Task analysis of “working” responses to dynamic interpretation in
short-term individual psychotherapy. Psychotherapy Research, 5,
49-62.
Jung, C. G. (1946). The psychology of the
transference. Collected works (Vol. 16). Princeton, NJ: Bollingen.
Jung, C. G. (1969a). Structure and
dynamics of the psyche. Collected works (Vol. 8). Princeton, NJ:
Princeton University Press.
Kahn, M. (1997). Between therapist and
client: The new relationship (Revised edition). New York: Internet Universities Press
Kantrowitz, J. (1997). A different
perspective on the therapeutic process: The impact of the patient on the
analyst. Journal of the American Psychoanalytic Association, 45, 127-153.
Kernberg, O. F. (1987). An ego
psychology-object relations theory approach to the transference. Psychoanalytic
Quarterly, 56, 97-221.
Kernberg, O. W. (1975). Borderline
conditions and pathological narcissism. New York: Jason Aronson.
Kiesler, D. J. (1982b). Confronting the
client-therapist relationship in psychotherapy. In J.C. Anchin & D. J.
Kiesler (Eds.), Handbook of interpersonal psychotherapy (280-295).
New York: Pergamon Press.
Klein, M. (1952). The origins of
transference. International Journal of Psycho-Analysis, 33, 433-438.
Langs, R. (1979). The interactional
dimension of countertransference. In L. Epstein & A. J. Feiner (Eds.), Countertransference (71-103). New York: Jason Aronson.
Lasky, R. (1990). Catastrophic illness and
the analyst's emotional reactions to it. International Journal of
Psycho-Analysis, 71, 455-473.
Lear, J. (1993). An interpretation of
transference. International Journal of Psycho-Analysis, 74, 739-755.
LeDoux, J. (1995). Emotion: Clues from the
brain. Annual Review of Psychoanalysis, 46, 209-235.
LeDoux, J. (2002). Synaptic self: How
our brains become who we are. New York: Viking.
Levin, F. (1997). Integrating some mind
and brain views of transference: The phenomena. Journal of the American
Psychoanalytic Association, 45, 1121-1151.
Levy, K., & Scala, J. (2012).
Transference-focused psychotherapies. Psychotherapy, 45, 391-403.
Lewis, H. B. (1987). Shame and the
narcissistic personality. In D. L. Nathanson (Ed.), The many faces of shame (93-132). New York: Guilford Press.
Lewis, M. (1995). Memory and
psychoanalysis: A new look at infantile amnesia and transference. Journal of
the American Academy of Child and Adolescent Psychiatry, 34, 405-417.
Lijtmaer, R. (2017). Variations on the
migratory theme: Immigrants or exiles, refugees or asylees. Psychoanalytic
Review, 104, 687-694.
Little, M. (1951). Countertransference and
the patient's response to it. International Journal of Psycho-Analysis, 32, 32-40.
Locke, E. & Latham, G. (2019). The development of goal setting theory: A half century retrospective. Motivation Science, 5, 93-105.
Looker, T. (1998). “Mama, why don’t your
feet touch the ground?: Staying with the body and the healing moment in
psychoanalysis.” L. Aron and F.S. Anderson (Eds.), Relational
perspectives on the body (237-262). Hillsdale, NJ: The Analytic Press.
Lyons-Ruth, K. (2000). I sense that you
sense that I sense … : Sander’s recognition process and the specificity of
relational moves in the psychotherapeutic setting. Infant Mental Health
Journal, 21, 85-98.
Main, R. (2004). The rupture of time: synchronicity and Jung’s critique of modern Western culture. New York: Brunner & Routledge.
Mandal, M., & Ambady, N. (2004).
Laterality and universality of facial expressions of emotions: The interface. Behavioural
Neurology, 15, 23-34.
Maroda, K. (1995). Projective
identification and countertransference interventions: Since feeling is first. Psychoanalytic
Review, 82, 229-247.
Matte Blanco, I. 1975). The unconscious
as infinite sets: An essay in bi-logic. London: Duckworth.
McLaughlin, J. (1990). Clinical and
theoretical aspects of enactment. Journal of the American Psychoanalytic
Association, 18, 595-614.
Meares, R., Stevenson, J., &
Comerford, A. (2005). Distinct pattern of P3a event and related in borderline
personality disorders. NeuroReport, 16, 289-293.
Meissner, W. (1996). The therapeutic
alliance. New Haven, CN: Yale University Press.
Miller, C. (2022). The object relations lens. New York: American Psychiatric Association.
Modell, A. H. (1980). Affects and their
non-communication. International Journal of Psycho-Analysis, 61,
259-267.
Montgomery, M., Luca, M., & Gordon-Finlayson, A. (2023). “The shifting sound of silence: A constructivist grounded theory. Counselling and Psychotherapy Research, 00, 1-11.
Nardi, A; Engelhard, E; & Or, M. (2023) Analyzing therapy logs: Mapping physical and mental manifestations of anxiety among children undergoing dance/movement psychotherapy. American Journal of Dance Therapy, 3,16-27.
Ogden, T. H. (1994). The concept of
interpretive action. Psychoanalytic Quarterly, 63, 219-245.
Ogle, C., Rubin, D., & Siegler, I.
(2012). The impact of the developmental timing of trauma exposure on PTSD
symptoms and psychosocial functioning among older adults. Developmental
Psychology, 49, 2191-2200.
Oschman, J. L., & Oschman, N. H.
(1995a) Somatic recall: Part 1–Soft tissue memory. Massage Therapy Journal,
34, 60-65.
Oschman, J. L., & Oschman, N. H.
(1995b) Somatic recall: Part 1–Soft tissue holography. Massage Therapy
Journal, 34, 66-74.
Pally, R. (2001). A primary role for
nonverbal communication in psychoanalysis. Psychoanalytic Inquiry, 21, 71-94.
Pearson, M. (1995). Problems with
transference interpretations in short-term dynamic therapy. British Journal
of Psychotherapy, 12, 37-48.
Perna, P. A. (1997). Reflections on the
therapeutic system as seen from the science of chaos and Complexity:
Implications for research and treatment. In F. Masterpasqua & P. A. Perna
(Eds.), The psychological meaning of chaos: Translating theory into practice (253-272). Washington, DC: American Psychological Association.
Pert, C. (1997). Molecules of emotion. New
York: Simon & Schuster.
Piaget, J. (1962). Play, dreams, and
imitation in childhood. New York: Norton.
Pick, I. B. (1985). Working through the
countertransference. International Journal of Psycho-Analysis, 66, 157-166.
Pick, I. B. (1997). Working through in the
countertransference. In R. Schafer (Ed.), The contemporary Kleinians of
London (348-367). Madison, CN: International University Press.
Piper, W. E., McCallum, M., Azim, H. F.
A., & Joyce, A. S. (1993). Understanding the relationship between
transference interpretation and outcome in the context of other variables. American
Journal of Psychotherapy, 47, 479-493.
Plakun, E. M. (1998). Enactments and the
treatment of abuse survivors. Harvard Review of Psychiatry, 5, 318-325.
Pollack, J., & Horner, A. (1985).
Brief adaptation-oriented psychotherapy. In A. Winston (Ed.).Clinical and
research issues in short-term dynamic psychotherapy (58-79).
Washington, DC: American Psychiatric Press.
Pribam, K. (1971). The Language of the
brain. Englewood Cliffs, NJ: Prentice-Hall.
Racker, H. (1953). A contribution to the
problem of counter-transference. International Journal of Psycho-Analysis,
34, 313-324.
Racker, H. (1968). Transference and
countertransference. New York: International Universities Press.
Racker, H. (1972). The meanings and uses
of countertransference. Psychoanalytic Quarterly, 41, 487-506.
Roth, P. (2001). Mapping the landscape:
Levels of transference interpretation. The International Journal of
Psychoanalysis, 82, 533-543.
Rothschild, B. (2000). The body
remembers: The psychobiology of trauma and trauma treatment. New York:
Norton.
Sampson, H. (1992). The role of
"real" experienced in psychopathology and treatment. Psychoanalytic
Dialogues, 2, 509-528.
Scaer, R. C. (2005). The trauma
spectrum: Hidden wounds and human resiliency. New York: Norton & Co.
Schacter, D., Curran, T., Ballucio, L.,
Milberg, W. P., & Bates, J. F. (1996). False recognition and the right
frontal lobe: A case study. Neuropsychologica, 34, 793-808.
Schaeffer, J. (2007). Transference and
countertransference in non-analytic therapy: Double-edged swords. New York:
University Press of America, Inc.
Schafer, R. (1975). Psychoanalysis without
psychodynamics. The International Journal of Psychoanalysis, 56, 41-55.
Schafer, R. (1976). A new language for
psychoanalysis. London, UK: Yale University Press.
Schafer, R. (1983). The analytic
attitude. New York: Basic Books.
Schafer, R. (1997). Vicissitudes of
remembering in the countertransference: Fervent failure, colonization and
remembering otherwise. International Journal of Psycho-Analysis, 78, 1151-1163.
Schore, A. N. (1994). Affect regulation
and the origin of the self. Hillsdale, NJ: Lawrence Erlbaum.
Schore, A. N. (2003a). Affect
dysregulation and disorders of the self. New York: W.W. Norton &
Company.
Schore, A. N. (2003b). Affect
regulation and the repair of the self. New York: W.W. Norton & Company.
Schore, A. N. (2011). The right brain
implicit self lies at the core of psychoanalysis. Psychoanalytic Dialogues,
21, 75-100.
Schwaber, E. (1990). Interpretation and
the therapeutic action of psychoanalysis. Journal of Psycho-Analysis, 71,
229-240.
Searles, H. (1975). The patient as
therapist to his analyst/Nontransference. In P. Giovacchini (Ed.), Tactics
and techniques in psychoanalytic therapy: Countertransference (Vol. II,
95-151). New York: Jason Aronson.
Shapiro, F. (1995). Eye movement
desensitization and reprocessing: Basic principles, protocols, and procedures. New
York: Guilford
Shapira-Berman, O. (2022). When should we not interpret? The analyst’s transformative act as a vital contribution to the patient’s sense of being real and alive. Psychoanalytic Perspectives, 19, 309-326.
Silberschatz, G. (2005). Transformative
relationships: The control-mastery theory of psychotherapy. New York:
Routledge.
Slochower, J. 1999. Erotic complications. International
Journal of Psycho-Analysis, 80, 1119-1130.
Smith, H. (1990). Cues: The perceptual
edge of the transference. International Journal of Psycho-Analysis, 71,
219-228.
Smith, H. (2000). Countertransference,
conflictual listening, and the analytic object relationship. Journal of the
American Psychoanalytic Association, 48, 95-128.
Spotnitz, M. (1976). Psychotherapy of
preoedipal conditions. New York: Jason Aronson.
Stark, M. (1994). Primer on working
with resistance. New York: Jason Aronson.
Stein, M. (1981). The unobjectionable part
of the transference. Journal of the American Psychoanalytic Association, 29, 869-891.
Stein, G. S. (1993). A transference
psychosis. Journal of Clinical Psychoanalysis, 2, 345-262.
Steiner, J. (1993). Patient-centered and analyst-centered interpretations: Some implications of containment and countertransference. In Psychic retreats: Pathological organization in psychotic, neurotic and borderline patients (402-422). London, U.K.: Routledge.
Stolorow, R. D. (1993). An intersubjective
view of the therapeutic process. Bulletin of Menninger Clinic, 57,
450-457.
Strachey, J. (1934, 1969). The nature of
the therapeutic action of psychoanalysis. International Journal of
Psycho-Analysis, 50, 275-291.
Strupp, H. H. (1989). Can the practitioner
learn from the researcher? American Psychologist, 44,717-724.
Sullivan, H. S. (1954). The psychiatric
interview. New York: Norton.
Swift, W. J., & Wonderlich, S. A.
(1990). Interpretation of transference in the psychotherapy of adolescents and
young adults. Journal of the American Academy of Child and Adolescent
Psychiatry, 29, 929-935.
Thornton, C. (2023). Lost boy who feared growing up. Psychodynamic Practice. Advanced online publication. http://dx.doi.org/10.1080/14753634.
Tmej, A., Fischer-Kern, M., Doering, S., Rentrop, M., Horz-Sagstetter, S., Buchheim, A. Borderline patients before and after one year of transference-focused psychotherapy (TFP): A detailed analysis of change of attachment representations. Society for Psychoanalysis and Psychoanalytic Psychology, 37, 1-10.
Tower, L. E. (1956). Countertransference Journal
of the American Psychoanalytic Association, 4, 224-255.
Treurniet, N. (1993). What is
psychoanalysis now? International Journal of Psycho-Analysis, 74,
873-891.
Tummala-Narra, P. (2019). The fear of
immigrants. Psychoanalytic Psychology. http://dx.doi.org/10.1037/pap0000245.
Vanaerschot, G. (1997). Empathic resonance
as a source of experience-enhancing interventions. In A. C. Bohart & L.
Greenberg (Eds.), Empathy reconsidered: New directions in psychotherapy (141-165). Washington, DC: American Psychological Association.
Van der Hart, O., Nijenhuis, E., et al.
(2006). The haunted self: Structural dissociation and the treatment of
chronic traumatization. New York: W.W. Norton.
Viederman, S. (1974). Interpretation in
the analytic space. International Review of Psychoanalysis, 1, 467-480.
Volkan, V. (1995) Six steps in the
treatment of borderline personality organization. Northvale, NJ: Jason
Aronson, Inc.
Wallerstein, J. (1990). Transference and
countertransference in clinical intervention with divorcing families. American
Journal of Orthopsychiatry, 60, 337-345.
Weiss, J., & Sampson, H. (1986). The
psychoanalytic process. New York: Guilford Press.
West, J. J., & Schain-West, J. (1997).
Envy in the countertransference. In M. J. Solomon and J. P. Siegel (Eds.), Countertransference
in couples therapy (126-135). New York: W. Norton & Company.
Wilkinson, M. (2003). Undoing trauma:
contemporary neuroscience. Journal of Analytical Psychology, 48, 235-243.
Wilson, A., & Weinstein, L. (1996).
The transference and the zone of proximal development. Journal of the
American Psychoanalytic Association, 44, 167-200.
Winnicott, D. W. (1949). Hate in the
counter-transference. In Collected papers. London: Tavistock.
Winnicott, D. W. (1960).
Countertransference. British Journal of Medical Psychiatry, 33, 17-21.
Winnicott, D. W. (1965). The
maturational processes and the facilitating environment. New York:
International Universities Press.
Winnicott, D. W. (1971). Playing and
reality. London: Tavistock.
Winston, A., McCullough, L., & Laikin,
M. (1993). Clinical and research implications of patient-therapist interaction
in brief psychotherapy. American Journal of Psychotherapy, 47, 527-539.
Wittig, R., Nessling, M., Will, R. D.,
Mollenhauer, J., Salowsky, R., Munstermann, E., Schick, M. Helmbach, H., Gschwendt,
B., Kom, B., Kioschis, P., Lichter, P., Schadendorf, D., & Poustka, A.
(2002). Candidate genes for cross-resistance against DNA-damaging drugs. Cancer
Research, 62, 22.
Wolstein, B. (1996). The analysis of
transference as an interpersonal process. American Journal of Psychotherapy,
50, 499-509.


 ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content.
ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content. ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027.
ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027. ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs.
ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs. ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.
ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.